Fibrodysplasia ossificans progressiva (FOP) is a rare genetic condition where bone gradually replaces muscles and connective tissues. Injury or illness causes new bone growth, which can be painful and lead to a shortened lifespan.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
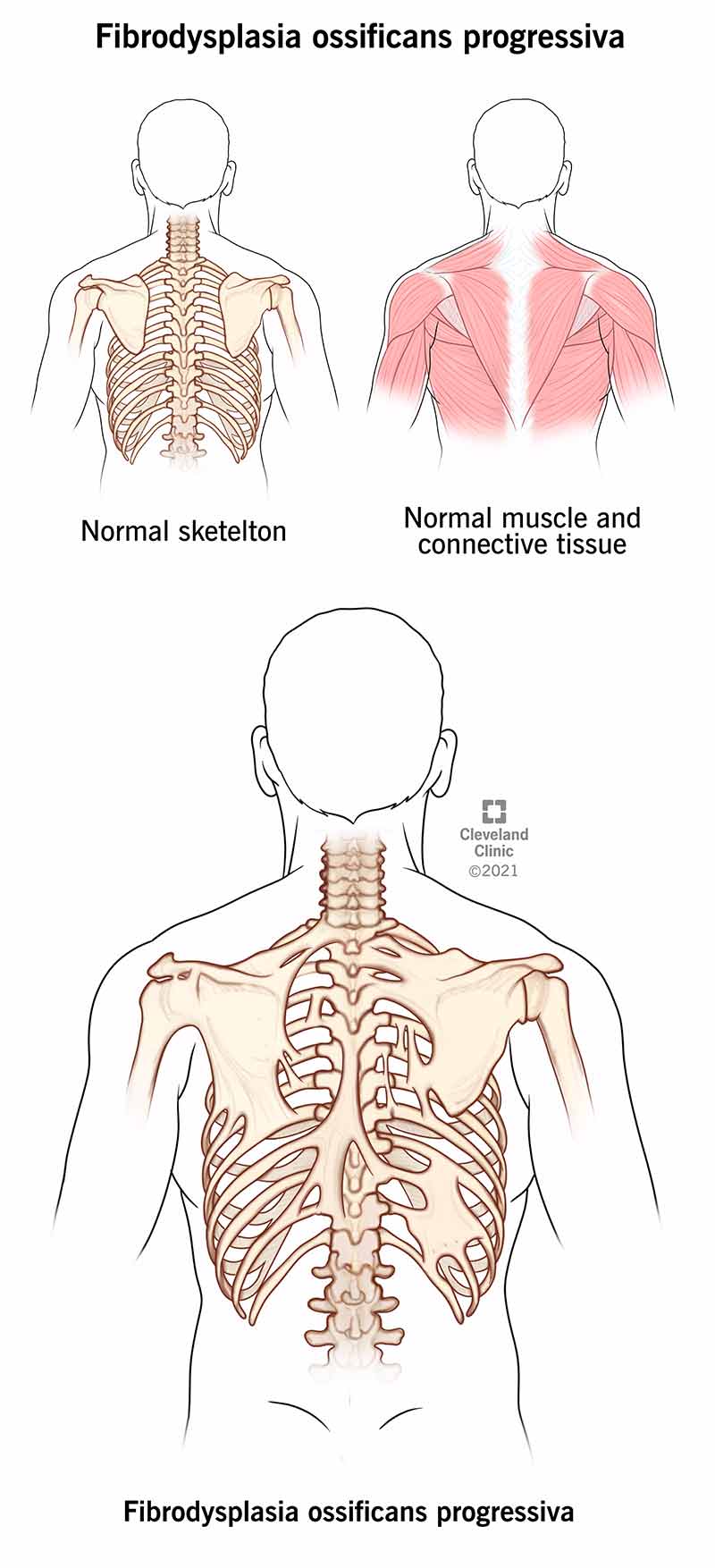
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24476-fibrodysplasia-ossificans-progressiva)
Pronunciation for the genetic condition fibrodysplasia ossificans progressiva is “fi-bro-dis-play-see-ah os-sif-eh-cans pro-gres-see-vah.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Fibrodysplasia ossificans progressiva (FOP) is a genetic condition where people are born with bunions and their body’s muscle tissue and connective tissues, like tendons and ligaments, turn into bone on the outside of their skeleton. This condition restricts movement and can cause a loss of mobility over time in people diagnosed with the condition. Symptoms of FOP appear during childhood and usually begin at the neck and shoulders before moving to other areas of the body.
Fibrodysplasia ossificans progressiva can affect anyone because it’s most often the result of a new genetic mutation that wasn’t inherited from a parent. Genetic mutations are unpredictable. They occur during fertilization due to an error when cells divide and replicate. Outside factors like smoking and chemical exposure can increase your risk of having a child with a genetic mutation, but if you plan on becoming pregnant, talk to your healthcare provider about genetic testing to assess your risks of having a child with a genetic condition.
Fibrodysplasia ossificans progressiva is a very rare condition that occurs in an estimated 1 out of every 2 million people worldwide.
People diagnosed with fibrodysplasia ossificans progressiva have a restricted range of motion due to their muscles and connective tissue gradually turning into bone. Signs of the condition start in the neck and shoulders as a child before moving downward to other parts of their body. Any type of trauma to the body can cause a flare-up of the condition. This could be after surgery, a fall or an illness (like the flu). These trigger swelling and inflammation of the muscles (myositis) that lasts for days to months around the affected area.
Advertisement
Children may experience difficulty eating (malnutrition) and speaking because irregular bone growth causes the mouth to not open completely. Extra bone growth around the rib cage can restrict how lungs expand and cause breathing difficulties.
Early cases of fibrodysplasia ossificans progressiva emerged in the 17th and 18th centuries where physicians first documented their findings. The condition received the name “myositis ossificans progressiva,” which means, “muscle turns progressively to bone,” in the early 1900s. After extensive genetic research by Dr. Victor McKusick of Johns Hopkins University School of Medicine, the condition’s name changed to fibrodysplasia ossificans progressiva to better reflect how both soft tissue and muscle turn to bone. In 2006, a research team at the University of Pennsylvania School of Medicine identified the specific genetic mutation that causes the condition.
A mutation of the ACVR1 gene causes fibrodysplasia ossificans progressiva. The ACVR1 gene gives your body instructions to make type 1 receptors for a protein called bone morphogenic protein (BMP) that reside in your muscles and cartilage. BMP controls how bones and muscles grow and develop. The mutation of ACVR1 causes symptoms of fibrodysplasia ossificans progressiva because the receptor, like a light switch, is always on when it should turn off.
Fibrodysplasia ossificans progressiva is an autosomal dominant condition, which means only one biological parent needs to pass the altered gene to the child for them to inherit it. If a parent has the gene that causes fibrodysplasia ossificans progressiva, there’s a 50% chance that the child will inherit the condition.
Most cases of fibrodysplasia ossificans progressiva occur because of a new mutation of the ACVR1 gene (de novo). This happens randomly, and there’s no link to the gene being present in a person’s family history.
The main symptom of fibrodysplasia ossificans progressiva (FOP) is the gradual replacement of muscles, tendons and ligaments into bone (heterotopic ossification). This process begins at the neck and shoulders in early childhood and progresses throughout the body over time. The development of bone can be rapid in some cases, or very slow in others. Each case is unique.
Symptoms arise during flare-ups, which are your body’s reaction to trauma that could be from an injury, surgery or viral illness like the flu. Swelling, or an increase in size or shape of a part of the body, can be painful. When flare-ups occur, the bone morphogenic protein type 1 receptors fail to stop producing proteins, which causes new bone to form on muscles, tendons and ligaments. After new bone forms, swelling decreases, which could take anywhere from a few days to a month.
Advertisement
A symptom of the condition that leads to an FOP diagnosis is a malformed and short big toe that sometimes grows inward and over the second toe. Growth differences of the big toes are visible at birth, even before other symptoms appear. Nearly 50% of cases of FOP also have malformations of the thumbs similar to the big toe.
Symptoms of fibrodysplasia ossificans progressiva include:
As the condition progresses, people diagnosed with FOP may permanently lose the ability to move. They may experience pain and stiffness caused by bone growths that pinch nerves. At this point in a person’s diagnosis, they may be more susceptible to respiratory infection or heart failure.
In severe cases of FOP, people might experience challenges with their cognitive function and ability to learn.
Diagnosis of fibrodysplasia ossificans progressiva begins with a physical examination that identifies the symptoms of the condition, along with reviewing your medical history and performing a genetic test, which is a blood test to identify the gene mutation that causes symptoms. Imaging tests like an X-ray help your healthcare provider examine new bone growth over muscle and connective tissue.
Advertisement
Diagnosis of fibrodysplasia ossificans progressiva can be challenging for healthcare providers. It’s possible to misdiagnose symptoms of FOP as cancer, juvenile fibromatosis (tumors or skin lesions form on soft tissue) or fibrous dysplasia. This occurs because FOP is extremely rare and very few healthcare providers encounter it during their careers. A biopsy of an FOP tumor — when your healthcare provider removes a small portion of the tumor to examine the cells under a microscope — often looks similar to a cancerous tumor.
If your healthcare provider suspects an FOP diagnosis, they won’t perform a diagnostic biopsy because the procedure can cause severe bone growth flare-ups. The most important symptoms that lead to an FOP diagnosis are malformed big toes and soft tissue swelling that forms throughout the body.
Treatment for fibrodysplasia ossificans progressiva aims to reduce symptoms, especially flare-ups that ignite the bone-growing process. There’s no cure for FOP but research and clinical trials are progressing to help people diagnosed with the condition. Treatment is unique for each person to address their specific symptoms.
Treatment for FOP could include:
Advertisement
Fibrodysplasia ossificans progressiva is a lifelong condition with no cure. The prognosis (outlook) is poor due to severe symptoms of the condition, including respiratory infections and restricted mobility that becomes worse over time. Life expectancy for someone diagnosed with fibrodysplasia ossificans progressiva is reduced into early adulthood. Most people are completely immobile by age 30. The most common cause of death among people with an FOP diagnosis is a respiratory infection. Research and clinical trials for new treatment options are in progress to help reduce symptoms and prolong the life of people diagnosed with the condition.
Preventing symptoms of fibrodysplasia ossificans progressiva involves avoiding trauma to your muscles and tissues. Symptoms flare up when you experience an event that causes stress to your body, like surgery, an injury or an illness. You can reduce your risk of having flare-ups of fibrodysplasia ossificans progressiva symptoms by:
You can’t prevent fibrodysplasia ossificans progressiva from occurring because it’s the result of a genetic mutation. To understand the risks of having a child with a genetic condition, talk with your healthcare provider about genetic testing.
After a fibrodysplasia ossificans progressiva diagnosis, work closely with your healthcare provider to find a treatment plan that’s unique to you and your symptoms. A genetic counselor can help you understand the diagnosis and provide emotional support for you and your family. Flare-ups of the condition may cause pain and discomfort, but your healthcare provider will offer options to ease symptoms.
You should visit your healthcare provider if:
If you have trouble breathing, contact 911 or visit the emergency room immediately.
After receiving a rare genetic diagnosis, you may be asking yourself, “What do I do next?” Your healthcare provider will monitor your health regularly and offer additional support. They may recommend you see a genetic counselor or an occupational therapist to help you better understand your diagnosis, minimize flare-ups and ultimately lead a comfortable life. Clinical trials and research are progressing to offer additional support to people diagnosed with the condition.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
