Urethral prolapse is when the inner lining of your urethra (the hole you pee from) sticks out. The condition mostly affects postmenopausal women and prepubescent girls. Symptoms may include pelvic pain, vaginal bleeding or pain when you pee. Treatment may be surgical or nonsurgical.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
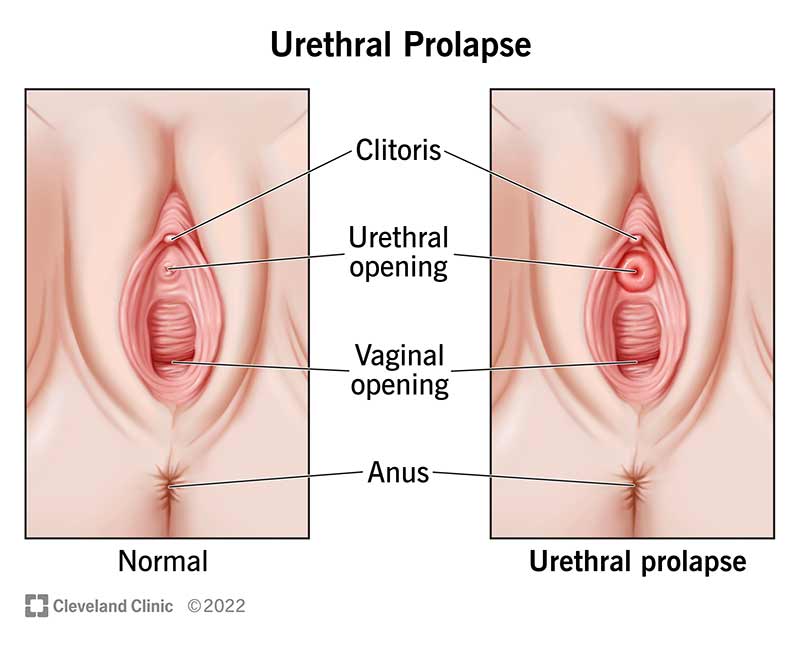
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24177-urethral-prolapse)
Urethral prolapse occurs when your urethra (the hole you pee from) protrudes (sticks out). When this happens, the area around your urethral opening may look like a tiny pink, red or purple ring.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your healthcare provider may use the terms urethral prolapse and urethral caruncle interchangeably. Specifically, urethral prolapse is when your urethra sticks out on all edges. A urethral caruncle forms when only one edge of your urethra sticks out.
Urethral prolapse is most common in postmenopausal women and prepubescent girls.
The condition is extremely rare in men. In the medical literature, there’s only one reported case of a prolapsed urethra in a male.
Urethral prolapse is rare. Most cases occur among the pediatric population — in about 1 out of every 3,000 children.
In most cases, urethral prolapse is mild and symptoms go away on their own. However, in severe instances, the prolapse may not receive enough blood supply, causing severe pain. For this reason, you should seek treatment for urethral prolapse as soon as you know it’s an issue.
The most common symptom is a visible ring of tissue sticking out of your urethral opening (this looks like a pink, red or purple donut). Some people with urethral prolapse don’t develop any symptoms at all. However, other urethral prolapse signs and symptoms include:
Advertisement
Experts don’t know exactly why some people get urethral prolapse. But, estrogen levels seem to play a role after menopause. You're more likely to develop the condition if you have low estrogen. For young girls, constipation and genetics are risk factors. Other risk factors include:
Typically, your urethra can be difficult to find because it’s so small. However, if you have urethral prolapse, the opening of your urethra is easier to find since it may be sensitive and swollen.
Your healthcare provider can diagnose urethral prolapse during a routine pelvic exam. Many people don’t even know they have a prolapsed urethra until their provider finds it and tells them about it.
Your healthcare provider may recommend surgical or nonsurgical urethral prolapse treatment, including estrogen cream, home remedies, antibiotics or surgery.
Because urethral prolapse is often associated with low estrogen levels, topical estrogen cream is a common treatment option. Applying a small amount daily can help strengthen the tissues that support your urethra.
Healthcare providers will monitor children using estrogen cream to minimize side effects like the development of pubic hair and breast budding.
In mild cases, you can treat urethral prolapse with simple home remedies, such as sitz baths to keep the area clean. Many people also apply petroleum jelly to ease tenderness and protect the area from irritation.
If you know the underlying condition that contributed to urethral prolapse, treating it can help you feel better soon. For example, treating constipation in children can prevent straining while pooping. As a result, the tissue can heal properly.
Sometimes urethral prolapse results in an infection. When this happens, your provider will prescribe antibiotics.
If your prolapsed urethra is severe — or if it has caused a blockage — then your healthcare provider may recommend surgery. During this procedure, your surgeon removes the tissue that’s sticking out and stitches the urethral lining back together.
If you receive nonsurgical treatment for urethral prolapse, the problem usually goes away within two weeks. If you need surgery, recovery could take up to six weeks. Your healthcare provider can tell you what to expect in your specific situation.
Advertisement
If you have urethral prolapse, your healthcare provider will discuss your treatment options with you in detail. Before recommending surgery, your provider will likely try to manage your condition with estrogen cream or other nonsurgical treatments. If urethral prolapse returns after treatment, surgery may be an option.
It’s possible for urethral prolapse to recur (return), even after successful treatment. You can reduce your risk of recurrence by avoiding additional pressure in your pelvic area. To do this:
Yes, it’s possible. Most mild cases of urethral prolapse get better with time. However, if your case is severe, surgery may be necessary.
If you think you might have a prolapsed urethra — or if you develop vaginal bleeding, pain when you pee, pelvic pressure or other symptoms — schedule an appointment with your healthcare provider. They can confirm your diagnosis and recommend treatment to ease your discomfort.
Urethral prolapse isn’t that common — and it’s usually not dangerous. But, when it does occur, it can lead to uncomfortable symptoms like vaginal irritation, pain when you pee or achiness in your pelvic area. While urethral prolapse is usually treated with nonsurgical methods, severe cases may require surgery. Your healthcare provider can help determine what caused your urethra to prolapse and recommend a treatment option that works for you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a condition that’s affecting your urinary system, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
