Klippel-Feil syndrome (KFS) is a condition in which you have two or more neck bones (vertebrae) fused together. KFS causes spine abnormalities and can affect many other body areas. Symptoms include short neck, limited neck mobility and low back-of-head hairline. Treatment depends on severity of your symptoms. Treatments range from devices to protect your spine to surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
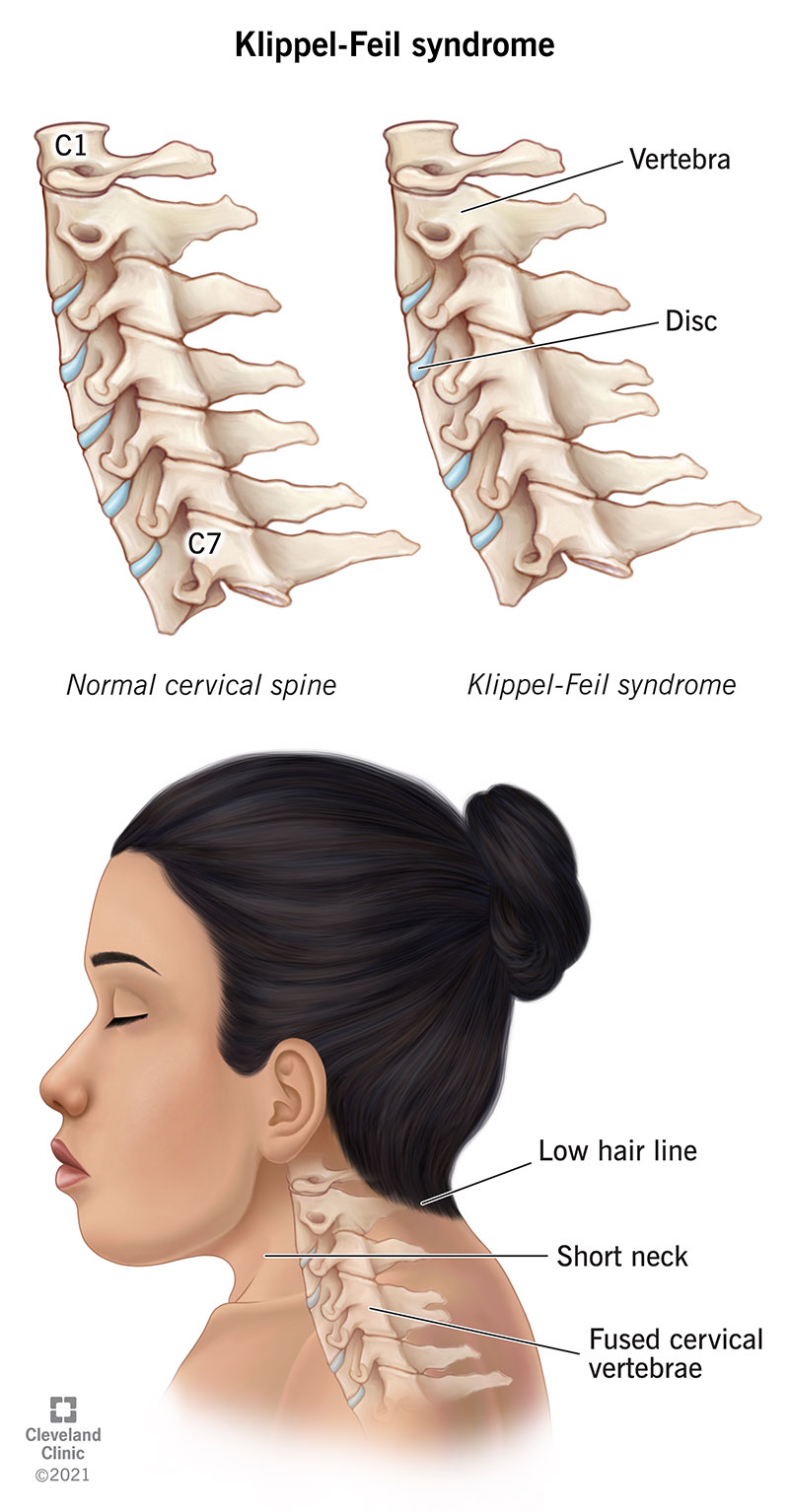
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23919-klippel-feil syndrome)
Klippel-Feil syndrome (KFS) is a rare condition in which two or more of the bones in your neck are fused (abnormally joined) together. These bones are called cervical spine vertebrae. This can also affect other vertebrae in your spine beyond the neck region.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This may involve many other parts of your body, including your heart and lungs, kidneys, mouth, eyes and ears, muscles and nerves, spinal cord and other bones.
Your spine consists of 33 vertebrae. The first seven vertebrae are called your cervical vertebrae, with C1 being closest to the base of your skull, and C7 being the last vertebra in this section. KFS most commonly affects your C2 and C3 vertebrae. Normally, each vertebra is separated by intervertebral disks and cartilage, which adds a cushion between vertebrae and allows them to slide against each other. If you have KFS, some of your vertebrae stick together like a single piece of bone.
The three most common physical features of KFS (you may have none, one or more of these) are:
KFS is a congenital condition, which means it’s something you’re born with.
The syndrome is named for the two physicians who first discovered the condition in the early 1900s.
Klippel-Feil syndrome (KFS) happens in about 1 in 40,000 to 42,000 newborns worldwide. It’s slightly more common in females.
Depending on the severity, Klippel-Feil syndrome (KFS) may be visible on ultrasound in the first trimester of pregnancy. If your provider can’t see it during pregnancy and there aren’t any obvious abnormalities at birth, during infancy or childhood, they may not discover it until the teen years or later. Late discovery is rare, however, because of the number of possible symptoms and abnormalities.
Advertisement
Occasionally, people with Klippel-Feil syndrome (KFS) have few or no symptoms. Most people, however, do have symptoms, which range from mild to severe. Symptoms vary greatly from person to person.
Common signs and symptoms include:
Other problems include:
Researchers don’t fully know what causes Klippel-Feil syndrome (KFS). Most cases are thought to be sporadic — meaning there’s no family history or obvious genetic cause. In others, changes (mutations) in one of the genes involved in bone and spine development cause the syndrome.
KFS can sometimes also be seen with another disorder or be a side effect of another congenital disease. If it’s a side effect of another congenital disease, KFS happens because of mutations in the genes involved in those disorders.
Some of these medical issues and conditions are:
In most cases, Klippel-Feil syndrome (KFS) isn’t inherited. However, in some cases, mutations in one of three identified genes cause this syndrome. When gene mutation(s) cause KFS, you can inherit the syndrome.
Advertisement
A healthcare provider makes the diagnosis of Klippel-Feil syndrome (KFS) based on your symptoms, a clinical exam and imaging studies. Providers usually diagnose this syndrome in childhood, and can sometimes even see it in a fetus before birth.
Your healthcare provider will ask about your medical history and family history and perform a physical. During the physical exam, your provider will:
There aren’t any lab tests that diagnose KFS, but your provider may order laboratory tests to rule out other conditions if you have multiple symptoms. They’ll examine your heart, kidneys and organs of the gastrointestinal tract and urinary tract for abnormalities. They may order a hearing test. Your provider may also discuss genetic testing.
Your healthcare provider will want to see X-rays, and maybe a computed tomography (CT) scan or magnetic resonance imaging (MRI).
Advertisement
Your symptoms determine the treatment. Treatment might include medications and/or physical therapy. You’ll need to understand any risks you have if you’re involved in trauma so you can avoid dangerous activities. Most people with KFS don’t need surgery.
The majority of people who don’t need surgery do well with conservative treatments such as using cervical collars, braces and traction. Your provider may order medications to relieve pain and inflammation.
You’re more likely to need surgery if:
If you have one or more fused cervical vertebrae below C3, close monitoring may be all that’s needed. If you or your child play contact sports, such as hockey or rugby, your healthcare provider may say you can continue to play these sports once you’ve learned how to protect your neck.
Advertisement
If you have any fused cervical vertebrae above C3 (nearest the base of your skull), you should avoid playing contact sports. You’re at greater risk of a dangerous spinal injury.
Your healthcare provider will regularly check your heart and lungs, reproductive system, kidneys and other organs to catch any problems early, manage or treat any changes, or recommend any needed surgery.
Klippel-Feil syndrome (KFS) can worsen over time. If your spine is abnormal, you’re more likely to develop problems as you age, such as degenerative disk issues, which can cause pinched nerves, pain in your back and spine or weakness in your arms or legs.
You’re more prone to injury through falls and blows to your body. Other internal problems may develop over time. This is why it’s important to see your team of healthcare providers as scheduled. They’ll perform check-ups and any needed tests or imaging studies to determine or change treatment.
Diagnosing Klippel-Feil syndrome (KFS) early is key to managing or treating health problems with surgery or by nonsurgical methods and careful watching over time. By fixing abnormalities and following your healthcare provider’s instructions for protecting your spine, you can usually have a normal life expectancy.
Your outcome depends on what your disease looks like (what parts of you are affected) and any other related conditions. Each person is unique. Your healthcare team will discuss your case when they see you at regular intervals. Some people have no symptoms and others have a significant number of symptoms that lower their quality of life.
Your healthcare providers will discuss if you need to do anything to protect your spine, if you can play contact sports or if you need to make other lifestyle changes. They’ll also discuss any need for surgery.
The types of healthcare providers who might be involved in your care include:
Klippel-Feil syndrome (KFS) is a rare spinal condition in which two or more vertebrae in your neck join together. The syndrome may be associated with many other spine problems and many other parts of your body can be affected too. However, each person is unique. You may have a mild form of KFS and not have significant symptoms or you may have more severe health issues that require long-term management. Your team of specialists will be with you each step of the way.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
