Costochondritis is inflammation in your costochondral joints — the cartilage that joins your ribs to your sternum (breastbone). It can be scary to feel chest pain, especially if it’s on the same side as your heart. But costochondritis isn’t a heart attack sign and doesn’t usually cause any complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
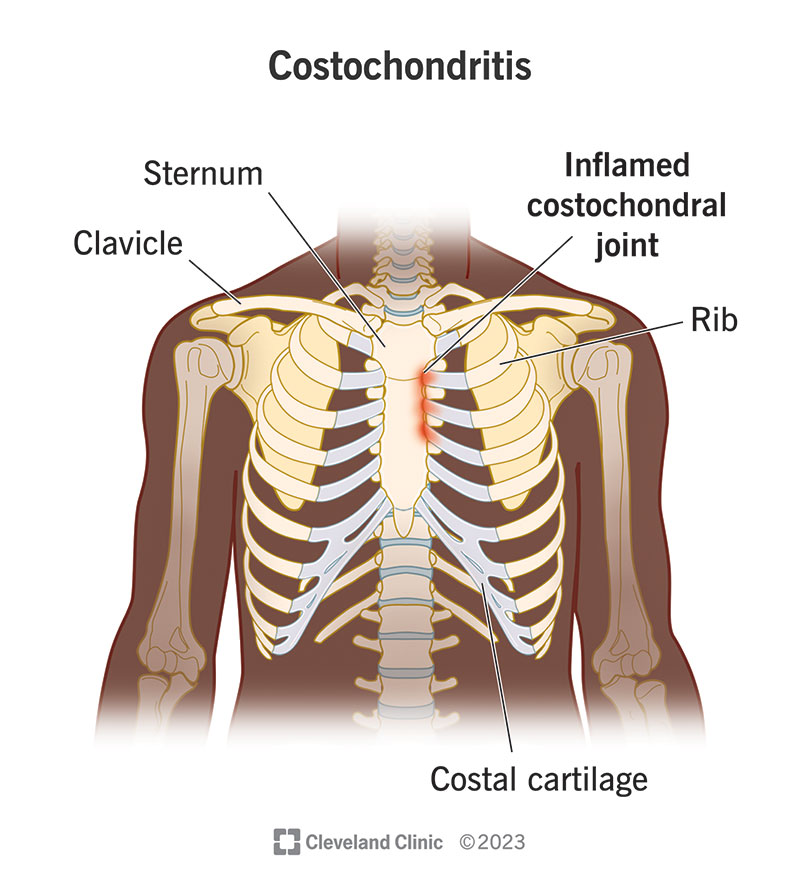
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/costochondritis)
Costochondritis is painful inflammation in the cartilage that connects your ribs to your breastbone (sternum).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those sections of cartilage are your costochondral joints. They’re stiff and strong to help your ribcage protect organs like your heart and lungs.
The inflammation can make breathing or moving your chest very painful. The pain can start suddenly or develop slowly and spread (radiate) across your chest.
Some people assume that any chest pain is a sign of a heart attack. But the same issues that cause heart attacks don’t cause costochondritis, and having costochondritis doesn’t mean you’re having a heart attack. But you should always visit a healthcare provider if your chest or ribs hurt, especially if the pain doesn’t get better in a few days.
Costochondritis is one of the most common causes of chest pain. Experts estimate that around one-third of people who visit a healthcare provider with chest pain or rib pain have costochondritis.
Chest pain is the most common costochondritis symptom.
Everyone experiences pain differently. Costochondritis usually feels like a low ache in your chest near your affected ribs. The pain might feel suddenly sharp or stabbing when you move your chest or torso. Some movements that can make costochondritis pain worse include:
Advertisement
Experts aren’t sure what causes costochondritis. Some experts think activities that put small, repeated stress on your ribs over time (microtraumas) can eventually trigger costochondritis. Microtraumas can include:
Anyone can develop costochondritis, but some people have a higher risk:
Costochondritis doesn’t usually cause any complications. It might be a sign that you have arthritis, especially ankylosing spondylitis.
Diagnosing costochondritis is usually a diagnosis of elimination. This means a healthcare provider might do an exam and perform tests to rule out other, more serious conditions before diagnosing costochondritis.
Your provider will diagnose costochondritis with a physical exam.
They’ll feel your chest and ribs. They might press on your chest to feel how sensitive you are and to pinpoint where your pain is most intense (localized). They’ll examine your torso for other signs of injuries or conditions that might be causing your symptoms.
You might need a blood test to check for infections or other issues.
There’s no imaging test that can diagnose costochondritis. But your provider may use some imaging tests to rule out other causes of rib pain. The most common tests include:
The most common costochondritis treatment is resting your chest and ribcage. Giving your irritated costochondral joints time to heal is the best thing to do for costochondritis.
Over-the-counter (OTC) medications like NSAIDs (nonsteroidal anti-inflammatory drugs) or acetaminophen can relieve your pain. Talk to your provider before taking pain medication for more than 10 days in a row.
It’s rare, but your provider might inject a corticosteroid into your affected joints to reduce the inflammation if your symptoms aren’t improving after a few weeks.
Some people with costochondritis get better without treatment, but don’t assume it’ll go away on its own. Visit your provider as soon as you notice any type of chest pain.
You should expect to make a full recovery from costochondritis. Once the inflammation heals, you should be able to return to all your usual activities with no long-term effects.
Advertisement
The worst part of costochondritis is usually the chest pain that makes people think they’re having issues with their hearts. Get new symptoms examined right away to rule out something more serious.
Costochondritis is usually a short-term issue. Most people experience symptoms anywhere from a few days to a few weeks. It’s rare, but costochondritis can last for several months.
Most people start to gradually feel better as they rest and take over-the-counter pain medications. Talk to your provider if your rib pain isn’t getting better in a few weeks after you start treating costochondritis.
There’s a chance that costochondritis comes back (recurs), even after it heals.
You might not be able to prevent costochondritis because experts aren’t certain what causes it.
In general, avoid putting too much stress on your chest and ribs. Make sure to rest after intense physical activity to give your body time to recover.
Visit your provider right away if you notice any new symptoms or changes in or around your chest, especially new pain. Costochondritis usually isn’t dangerous, but it’s important to rule out other, more serious issues as soon as possible.
Call 911 (or your local emergency services phone number) or go to the ER if you think you’re experiencing heart attack symptoms, including:
Advertisement
Tietze syndrome is very similar to costochondritis. It’s another type of irritation in your costochondral joint.
The biggest difference between them is swelling and which ribs they usually affect.
Tietze syndrome causes pain, tenderness and swelling near affected costochondral joints. It usually affects ribs higher up on your ribcage, closer to your shoulders — usually your second or third ribs.
Costochondritis symptoms are almost identical to Tietze syndrome, except costochondritis doesn’t cause swelling that you can see or feel. It typically affects ribs lower down your ribcage — usually ribs two through five.
Because costochondritis and Tietze syndrome are so similar, they’re sometimes confused for each other. The good news is they’re usually treated and diagnosed the same way. Visit a healthcare provider if you have any pain or swelling in or around your chest.
Advertisement
Lots of conditions and injuries can cause rib pain. Other than costochondritis or Tietze syndrome, some rib pain causes can include:
Visit your provider if you have new symptoms in your ribs or chest. Costochondritis doesn’t usually cause breast pain or muscle pain.
Anything that makes breathing or moving hurt is annoying, and that’s even more true when that pain is in your ribs and chest. Fortunately, costochondritis usually isn’t dangerous or a sign of something serious. But that doesn’t mean the pain in your ribs isn’t real.
Visit a provider as soon as you feel any chest pain. They’ll help you understand what’s causing it, how you can help your body heal and what you should look out for as you recover.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
