Treacher Collins syndrome is a rare inherited group of conditions that affects the growth of a child’s skull and facial bones. It can cause facial differences and hearing loss. Treatment often includes reconstructive surgery. Without treatment, children with Treacher Collins syndrome can develop complications that require lifelong medical support.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
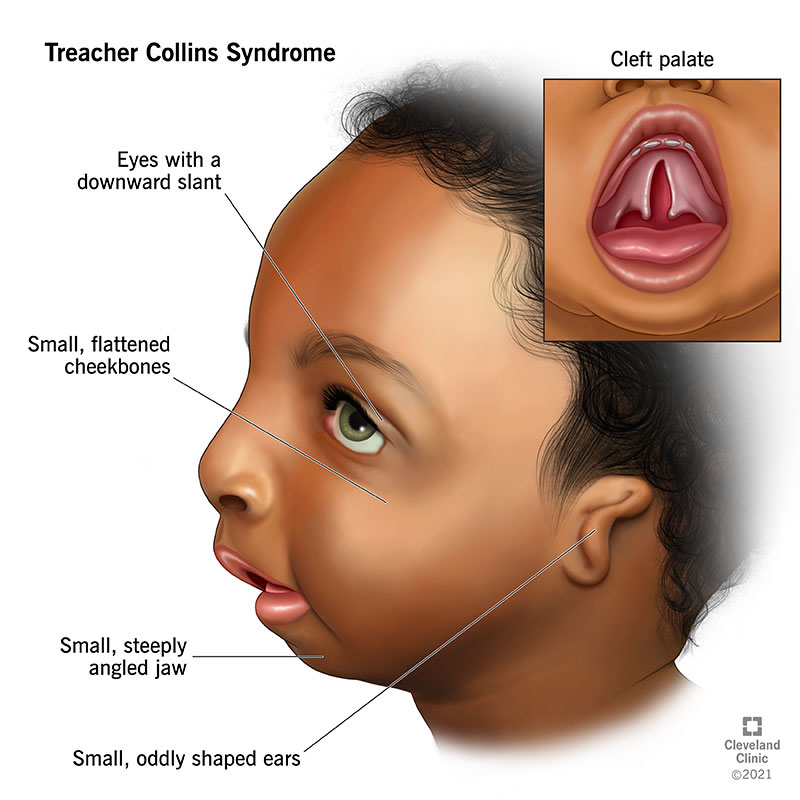
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22149-treacher-collins-syndrome)
Treacher Collins syndrome is an extremely rare inherited group of conditions that affect the size, shape and position of your child’s ears, eyes, cheekbones and jaws. The syndrome can cause one or more conditions that affect your child’s ability to nurse or bottle-feed, breathe easily or hear. Another name for Treacher Collins syndrome is mandibulofacial dysostosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your child’s symptoms can range from mild and almost unnoticeable to very severe. Most children who have Treacher Collins syndrome have surgery to correct facial differences like cleft palate. Some may need treatment for hearing loss, as well.
With treatment and routine healthcare follow-ups, children with Treacher Collins syndrome can live long, healthy lives. Early intervention is key, though. Without treatment, children with Treacher Collins syndrome may develop complications that require lifelong medical care.
Treacher Collins syndrome affects approximately 1 in every 50,000 children worldwide.
Children with Treacher Collins syndrome have distinctive facial characteristics, like:
Researchers link Treacher Collins syndrome to genetic variation. About half of all children who have the syndrome have a biological family member with the condition. But it also happens sporadically, with no apparent cause.
Children with Treacher Collins syndrome may have:
Advertisement
Healthcare providers might make a preliminary diagnosis based on regular newborn examinations. If your child’s symptoms point to Treacher Collins syndrome, your provider may refer you to a genetics specialist for further testing and diagnosis.
Treacher Collins syndrome treatment depends on your child’s specific situation and medical needs. Not all children born with the condition require the same care.
From infancy through childhood, the goal of treatment is to improve health and function. Early in life, your child may need surgeries to help them breathe better. Sometimes, this may include a tracheostomy. In addition, many children will need some type of reconstructive surgery. Once they’ve finished growing (usually in their late teens or early adulthood), some people may choose to explore cosmetic surgery options, as well.
Healthcare providers use reconstructive surgery to treat structural abnormalities, ease symptoms and improve your child’s health. Depending on your child’s situation, they may need surgery on their:
The condition itself isn’t curable. But surgery can correct complications like facial differences, breathing issues and hearing loss.
People with Treacher Collins syndrome typically have a normal lifespan if they get the treatment they need as children. Treatment and regular follow-ups can ease symptoms and improve quality of life. Without treatment, children can develop complications that require lifelong medical care.
Genetic changes cause Treacher Collins syndrome, so there’s no way to prevent it. If your family has a history of Treacher Collins syndrome, you might consider genetic counseling. This can help assess the risk of passing it down to your biological children.
Learning that your child has Treacher Collins syndrome can be scary. The uncertainty of the path ahead — like which treatments they might need — may feel overwhelming. But your healthcare provider is here to help. They’ll check in with you and your child regularly and give you a basic timeline for what treatment might look like.
The most important thing to remember is that Treacher Collins syndrome doesn’t interfere with your child’s ability to learn and be active. It has no effect on overall growth, brain development or intelligence. Encouraging your child to play, try new hobbies and explore the world around them can help them thrive.
Advertisement
You probably have questions about your child’s health, as well as questions about their appearance. Here are some questions you might consider asking your child’s healthcare provider:
It’s possible. Healthcare providers track fetal development with regular ultrasounds. Your child’s facial characteristics are usually visible via ultrasound by the beginning of your second trimester. Ultrasounds might reveal more severe forms of Treacher Collins syndrome, but this isn’t always the case.
Yes, people with Treacher Collins syndrome can have children. If you have Treacher Collins, there’s a 50% chance that your child will have it, too.
There’s no evidence that suggests Treacher Collins affects brain development or intellectual ability. Children with hearing loss may experience certain developmental delays, but treatments like hearing aids and speech therapy can help.
In our eyes, our children are perfect — and that’s how we want the world to see them. But Treacher Collins syndrome can make it difficult for the world to see our children as we see them.
Advertisement
There’s no cure for Treacher Collins syndrome, but healthcare providers have many ways to help. There are surgeries to ease breathing difficulties and hearing loss, as well as surgeries known as craniofacial reconstructions to help correct your child’s facial differences. Just as important, there are providers with experience and compassion who understand the journey you’re on — and they’ll walk with you every step of the way.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Treacher Collins syndrome is a rare genetic condition that can affect your child’s facial development. Cleveland Clinic Children’s team of experts is here to help.
