Osteochondritis dissecans (OCD) happens when a section of bone and cartilage in one of your joints loses its blood supply. This makes that piece soft and weak. Eventually, the affected section of bone might break loose. You may be able to treat OCD at home with rest and over-the-counter anti-inflammatory medications. Some people need surgery to repair the joint.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
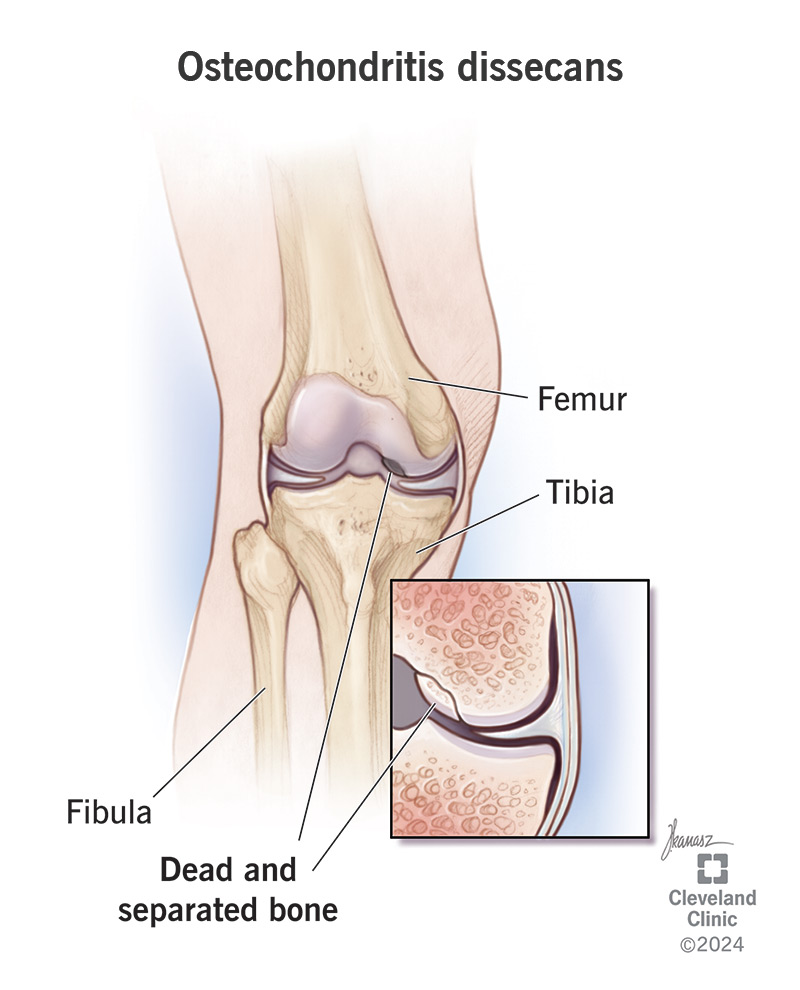
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/osteochondritis-dissecans)
Osteochondritis dissecans (OCD) is a condition that affects your joints. It usually develops in children, teens and young adults.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A joint is any place in your body where two bones meet. Osteochondritis dissecans affects the end of one bone in a joint. It cuts off blood supply to a section of the bone which makes it soften and weaken. Eventually, the affected section of bone dies and separates from the rest of your bone. This can pull some cartilage with it. OCD leaves a lesion (mark) where the bone and cartilage break off.
The loose bone and cartilage might remain in place or move into another area of your joint. This can make the joint unsteady or painful. You might not feel any symptoms for a long time. It can take months or even years for osteochondritis dissecans to develop.
OCD usually affects joints like your:
It’s most common to develop OCD in your knee, specifically at the inside edge at the bottom of your femur (thigh bone) — the medial femoral condyle.
There are two types of osteochondritis dissecans:
Advertisement
You might not experience symptoms early on or if the separated piece of bone and cartilage don’t drift far out of place.
If you do have osteochondritis dissecans symptoms, they can include:
These symptoms usually only happen if the piece of bone breaks off and drifts into other areas of your joint.
You might feel symptoms more often or more intensely during or after physical activity or exercise.
Researchers are still studying sporadic osteochondritis dissecans and haven’t been able to find or prove one single cause. Because it’s more common in athletes, experts think repeated stress on a joint may cause OCD. Healthcare providers call these microtraumas — high-stress events that don’t damage a joint right away, but that can add up over time to cause injuries. Jumping, running and throwing can all cause microtraumas in your joints.
Familial osteochondritis dissecans is caused by a genetic change. A change in the ACAN gene causes familial OCD. The ACAN gene carries the code for your body to make a cartilage-building protein called aggrecan. The mutation causes your aggrecan to build weak or disorganized cartilage.
Anyone can develop OCD, but some people are more likely to, including:
Untreated osteochondritis dissecans can cause worsening symptoms over time. Eventually, you might develop chronic pain or arthritis.
If you have familial OD, you’re more likely to develop osteoarthritis much earlier than usual (when you’re younger than 50).
A healthcare provider will diagnose osteochondritis dissecans with a physical exam and imaging tests.
They’ll examine your affected joint and ask about your symptoms. Tell your provider when you first noticed symptoms like pain and stiffness, or if any activities seem to make them worse.
Your provider will check your range of motion and compare it to your other, unaffected joints — one knee against the other, for example.
Your provider will use X-rays or an MRI (magnetic resonance imaging) to take pictures of your joints. You might need genetic testing to confirm or rule out familial OCD.
Your provider will suggest treatments that help your joint heal and restore blood flow to your affected bone. The most common OCD treatments include:
Advertisement
Your provider might suggest surgery if you’ve tried other treatments and still have severe symptoms after a few months.
Your surgeon might:
Which type of surgery you need depends on which joint has OCD, how severe the damage is and how far out of place the detached tissue is. Your surgeon will tell you what to expect.
The term “natural” doesn’t have a set medical definition. Most people can manage osteochondritis dissecans symptoms with conservative or at-home treatments. Remember, there’s nothing “unnatural” about needing medication or surgery to treat a medical condition, including OCD. The best treatment for you is the one that works and helps your joint heal.
Kids and teens with osteochondritis dissecans are more likely to heal with only rest and time.
But don’t take a chance with your child’s joints. Visit a healthcare provider if your child has joint pain or other symptoms for more than a week.
Advertisement
The sooner a provider diagnoses and treats a joint issue, the less likely it is your child will experience complications.
Most people need a few months to heal. Your provider will tell you which kinds of physical activities are safe to do while you’re recovering.
Recovering from osteochondritis dissecans surgery usually takes around two months. You’ll need physical therapy for a few months after that to regain your strength and range of motion.
Kids and teens usually don’t have long-term effects after a provider diagnoses and treats osteochondritis dissecans.
Your child might have to change sports or avoid certain repetitive motions to prevent future joint injuries. For example, some kids with OCD in their elbows can resume playing baseball once they’ve healed, but they have to avoid pitching.
Adults have a higher risk of developing osteoarthritis in their affected joints and are more likely to need OCD surgery.
Osteochondritis dissecans usually doesn’t come back (recur) once you’ve healed. But you’re more likely to develop OCD again in the future if you have familial OCD.
You probably can’t prevent osteochondritis dissecans because experts aren’t sure what causes it. The best way to take care of your joints is to maintain good overall health, including:
Advertisement
Talk to your provider about genetic screening if one of your close biological relatives (like a biological parent or grandparent) has OCD.
Visit a healthcare provider if you have joint pain that lasts for more than a week. Go to the emergency room if you experience a trauma or can’t move a joint.
You may want to ask your provider:
Osteochondritis dissecans happens when a section of bone in one of your joints loses its blood supply and becomes soft and weak. Even though experts aren’t sure what causes it, your provider will suggest treatments to help your bones and joint heal. They’ll tell you which activities to avoid while you’re recovering, and when it’s safe to return to training, playing sports or doing more intense activities.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
