Lewy body dementia (LBD) is a decline in mental functioning that happens when clumps of proteins called Lewy bodies build up in your brain cells. They damage parts of your brain that affect thinking, behavior, movement and sleep. LBD gets worse over time. There’s no cure, but medications and therapies may help manage symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lewy body dementia (LBD) is a progressive brain disorder that happens when certain proteins called Lewy bodies build up in your brain cells. This makes it harder to think clearly and do everyday activities.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With this type of dementia, symptoms start slowly and get worse over time. There’s no cure, but your healthcare provider can help you manage symptoms with medications and therapies.
According to the U.S. National Institute on Aging, Lewy body dementia affects more than 1 million people in the United States. In adults after age 65, LBD is the second most common form of dementia after Alzheimer’s.
There are two types of LBD. They have similar symptoms. The difference is when the cognitive and movement problems begin:
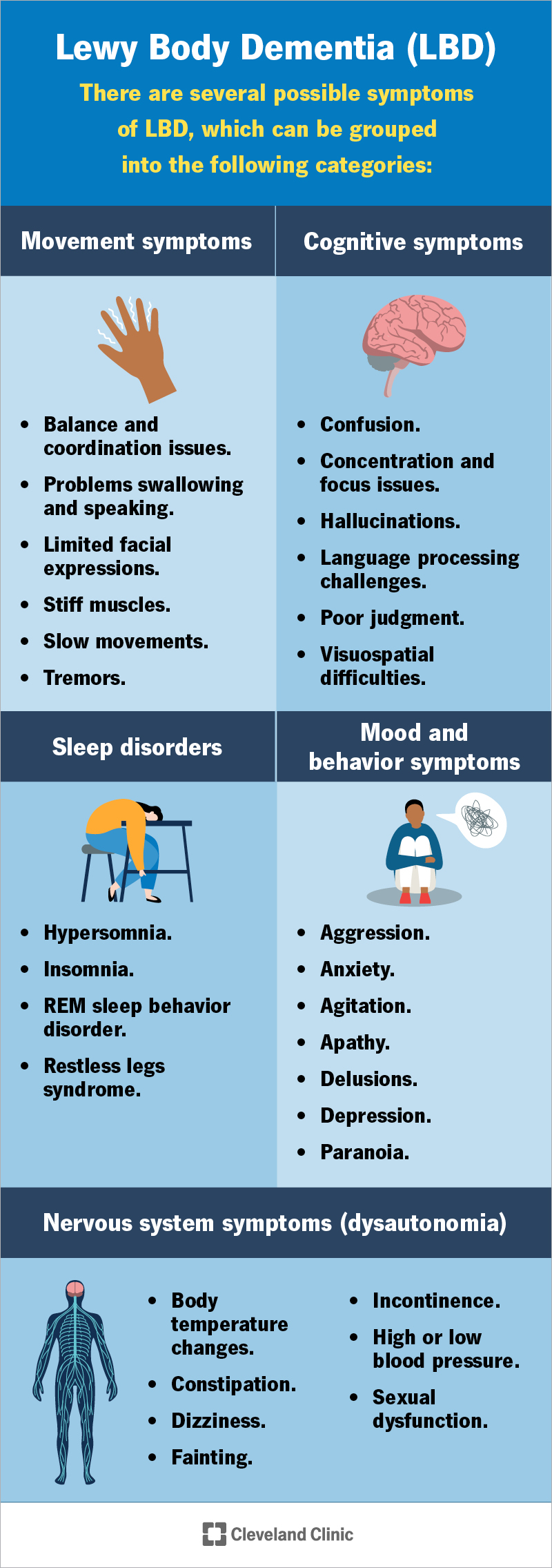
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17815-lewy-body-dementia)
LBD causes a mix of symptoms. They can be different for each person:
Advertisement
Symptoms may come and go. Some start early (acting out dreams or loss of smell) or show up later. They’ll slowly get worse over time.
Your provider may describe LBD in stages. These stages show how thinking and movement abilities change over time.
LBD happens when proteins called Lewy bodies (alpha-synuclein) build up in brain cells. These proteins damage parts of your brain that control thinking and memory.
Doctors and researchers don’t know why some people get LBD and others don’t.
LBD usually affects people after age 50. Having a biological family history of LBD or Parkinson’s disease can raise your risk.
Certain genes, like APOE and GBA, may also increase your chances. But having these genes doesn’t mean you’ll definitely get LBD.
Researchers are still studying other factors that may raise the risk of developing this condition.
LBD can lead to serious health problems, and some may be life-threatening:
Dementia can impact your mental health. If you’re feeling overwhelmed, are thinking about suicide or self-harm, call or text 988 in the U.S. This is the Suicide & Crisis Lifeline. Someone is there to talk to you 24/7.
To make a diagnosis, your provider may use the following steps:
A team of specialists may work together to make a diagnosis. This team might include:
They combine your test results and symptoms to determine if you have “probable LBD.” This means you most likely have the condition based on the information they have, even though there isn’t a single test that can say for sure.
There’s no cure for Lewy body dementia and no way to prevent it. But medications and therapies can help manage symptoms for a while.
Your doctors will look at how LBD is affecting you and what stage you’re in. Then, they’ll create a treatment plan that best fits your needs.
In later stages, your care team may focus more on palliative care. This means providing comfort, support and relief from symptoms instead of intense treatments or hospital stays.
Advertisement
Your provider may offer different medications. These can include:
Your provider may also recommend medications for nervous system symptoms, like dizziness or blood pressure changes when standing. These are usually prescribed if other steps, like raising your legs, eating foods with more salt or drinking more fluids, don’t help.
Different types of therapy may help, including:
LBD can also impact your mental health. Talking to a mental health professional, either one-on-one or in a group, can help you and your family cope. Support groups are also available to connect you with others going through similar experiences.
Advertisement
A calm and steady routine can be a benefit as well. This can prevent symptoms like confusion, agitation and stress.
Hallucinations are often one of the first signs of Lewy body dementia. If you or a loved one starts seeing things that aren’t there, especially with changes in movement, mood, behavior or thinking, talk to a healthcare provider.
If you’ve already been diagnosed with LBD, you’ll need regular check-ups. Your care team will track your symptoms, adjust treatments as needed and watch for any side effects. Be sure to tell them if anything changes or if new symptoms appear.
On average, people live five to eight years after being diagnosed with Lewy body dementia. However, this number can vary. Some people live much longer, sometimes even decades.
Your provider can help you understand what to expect. Everyone’s experience is different.
As this is a progressive disease, that means it gets worse over time. Some people decline slowly, while others may notice faster changes. Your general health and other medical conditions can affect how the disease progresses.
If you have LBD, your provider will suggest treatments to manage symptoms that improve your comfort and safety.
As the disease progresses, you may lose the ability to make decisions or handle daily responsibilities. That’s why it’s important to talk early about care planning. An advance directive is a smart step. It’s a legal form that tells others what care you want if you can’t speak for yourself.
Advertisement
Learning that you have Lewy body dementia (LBD) isn’t easy. You and your loved ones may worry about what’s ahead. But no one can predict exactly how the disease will progress. The best approach is to take things one day at a time.
While the symptoms can be unpredictable, there are ways to manage them. Treatments, therapies and support systems can help you stay independent and keep up with daily life for as long as possible.
It also helps to build a care team you trust, keep a calm daily routine and talk about future plans while you’re still able to make decisions. These steps might seem big, but they’re really about making things a little easier for you and the people who care about you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Learning you could have Lewy body dementia can change your world. But Cleveland Clinic is here to help you and your family manage this brain disorder.
