A blocked tear duct means your tear fluid can’t flow out of your eyes properly. These blockages can cause disruptive symptoms like watery eyes or trouble seeing. And they also can increase the risk of an infection. Babies are most likely to get them, but adults can have them, too. Fortunately, most causes are treatable and reversible.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
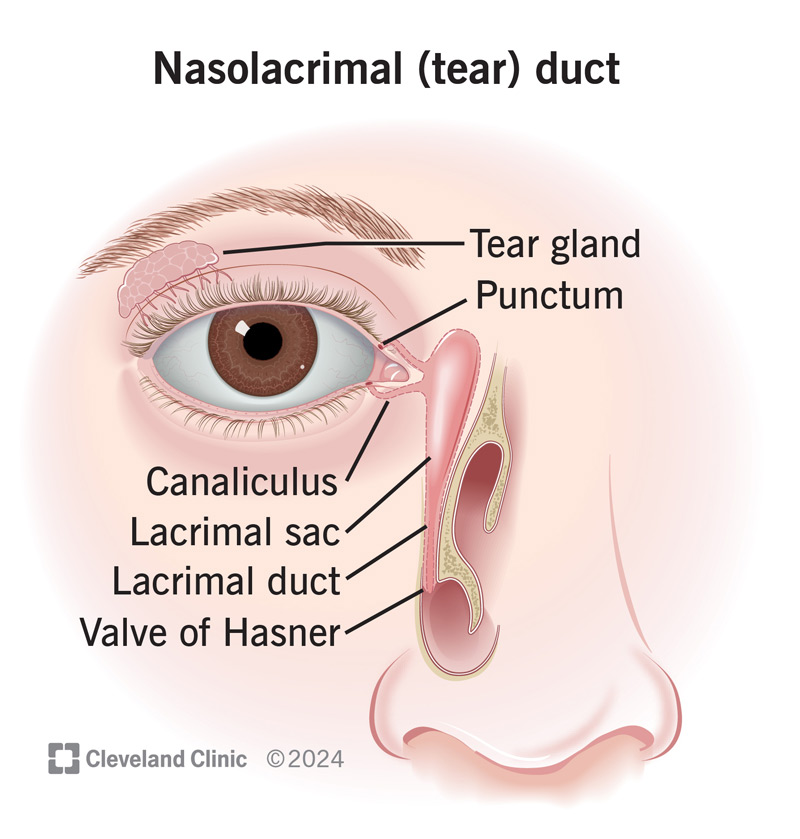
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/blocked-tear-duct-nasolacrimal-duct-obstruction)
A blocked tear duct is a condition that happens when something keeps tear fluid from draining out of your eyes properly. These blockages slow or stop the flow of tear fluid, causing it to back up in the tear duct system and into your affected eye. The medical term for this condition is “nasolacrimal duct obstruction.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your eyes need tear fluid to work properly. Your tear fluid lubricates the surface of your eye and helps your corneas absorb oxygen. Tear fluid also contains immune factors that protect against, or help your eyes recover from, infections.
You can think of your tear system like the gutters and downspouts on a house. The gutters channel water toward the downspout. But a blockage or clog in the downspout can make water back up and spill over the gutters’ edges.
The tear duct system is a series of openings and tubelike structures. The route that tear fluid follows to leave your eyes is:
Advertisement
Tear duct blockages are common in very young children, affecting between 6% and 20% of infants. They’re much less common in adults.
The symptoms of a blocked tear duct can include:
These blockages can also make it easier to develop infections in the tear ducts. Infection symptoms can include:
Tear duct blockages can happen for a few different reasons. Some are congenital, meaning you have them when you’re born. Others develop later in life.
Congenital tear duct obstruction usually happens because a child still has an unbroken membrane where the valve of Hasner should be. That means fluid can build up inside the lacrimal duct. Over time, the accumulated tear fluid can cause the duct to expand. It can also lead to an infection of the tear duct or other parts of the tear system.
Tear duct blockages can also happen because of other conditions or be more likely to happen under certain circumstances. These are more likely to happen higher up in your tear duct system (or in parts that aren’t technically tear ducts, but they connect to the ducts).
Examples include:
Advertisement
Babies have the highest chance of developing a blocked tear duct. Blockages usually happen because the membrane at the bottom of the tear nasolacrimal duct doesn’t open and become the valve of Hasner.
Adults are more likely to develop a tear duct blockage if they have a history of:
A blocked tear duct is just the kind of place where bacteria find it easy to grow, so bacterial infections or abscesses are the main possible complications of a blocked tear duct. The infections can also affect your sinuses, eyes and other nearby tissues. That’s why treating and keeping the infection from spreading is very important.
An eye care specialist or healthcare provider can usually diagnose a blocked tear duct based on your symptoms and by inspecting or feeling around your eye and tear duct. They’ll also ask you about your symptoms. If your baby might have a blocked tear duct, they can also check for this or do certain tests to look for a blockage.
One simple test they can do is called the “dye disappearance test.” To do it, a provider adds a drop of a special dye called fluorescein to your eye. Fluorescein glows under a blue light, so a provider can put a single drop of it into saline and then put the saline into your eye. After five minutes, they can check with a black light and see if any dye remains. If it’s still there, that can indicate you have a total or partial tear duct blockage.
Advertisement
Other tests are also possible, especially if your healthcare provider suspects that a blocked tear duct might be happening because of another condition or issue. The tests they recommend depend on your symptoms, circumstances and what condition they suspect could be the cause.
Because so many factors can play a role, it’s best to talk with them about the testing options. They can provide information that’s specific and relevant to your particular situation.
A blocked tear duct is very treatable. But the treatments are different depending on the age of the person who has it and other factors. This condition can get better without treatment, especially in babies, but it’s better to try and treat it to avoid complications like infections.
Some treatments, like antibiotics, are possible no matter your age. These are most likely if you have an infection related to a blocked tear duct, and they can come in topical or eye drop forms. Other medications may also help. Your eye care specialist is the best person to tell you more about these options.
The main treatment for babies and infants with a blocked tear duct is a special massage technique that you can do at home. If your child or a child you care for has it, their pediatrician can show you exactly how to do this. This massage technique is usually all it takes to make the membrane pop open and become a valve.
Advertisement
If the blockage doesn’t get better with massage by the time a child has their first birthday, it’s more likely they’ll need a different treatment approach. Massaging also isn’t likely to help adults, so other treatments are usually necessary.
Some of these treatments may need to happen under sedation or anesthesia. Your (or your child’s) eye care specialist or provider can tell you if and why they recommend sedation or anesthesia.
One of the simpler approaches to treating a blocked tear duct is a three-step technique called dilation, probing and irrigation. This technique can help babies if massage isn’t helpful. It’s also a likely first treatment for older children and adults.
The steps of the technique work like so:
In cases where simple dilation, probing and irrigation aren’t enough, a more advanced type of dilation may be necessary. When this is the case, your child’s eye care specialist will use a tool with a tiny balloon attachment on it. They’ll inflate the balloon slowly and gently in narrowed areas. Pushing like this from the inside can often widen the duct and resolve the issue.
In some cases, balloon dilation may not be enough to widen a narrow tear duct permanently. In these cases, inserting a tube or stent might be the best approach. These devices provide a sturdy, hollow framework that can hold the duct open and still let tear fluid flow through.
In some cases, surgery may be the best choice to fix a blocked tear duct or reroute tear fluid around it. Two main surgeries are possible:
The advantages, disadvantages and possible complications of the surgical procedures vary widely. The type of blockage you have, where it is and other factors can all play a role. Your surgeon or eye care specialist is the best source of information about what you can expect.
Tear duct blockages usually have a positive outlook, depending on why they happen. Tear duct blockages aren’t dangerous on their own. But some of the causes can be. And blockages can lead to dangerous infections, so getting a blockage diagnosed and treated is important.
Congenital blockages have an excellent outlook. About 70% of children with these blockages get better by the time they’re 6 months old, and 90% get better by their first birthday. While blockages can go away spontaneously, the massage technique speeds up that process and reduces the chance of an infection or other issues. Congenital blockages also usually don’t cause problems later in life.
In adults, the outlook is generally good, depending on the cause. Most causes, especially injury-related causes, respond well to treatment, and many approaches can help. Your eye care specialist can tell you more about which treatments are most likely to help, the outcome you can expect, and what you can do to improve that outcome.
Tear duct blockages happen for reasons that are unpredictable, outside your control or that you can’t see happening. That means there’s no way to prevent them.
There are a few things you can do to reduce the odds of an issue that could lead to a blockage, though. These mainly revolve around avoiding infections, including the following precautions:
If you have (or a child you care for has) a tear duct blockage, an eye care specialist can guide you on treating and managing it. You shouldn’t try to self-diagnose or self-treat a tear duct blockage. If you think you have symptoms of a blockage, you should schedule an appointment with an eye care specialist and see them as soon as possible.
If you have a tear duct blockage, your eye care specialist will give you treatment instructions and guidance. You can also ask them about the signs and symptoms that mean you need to call them or seek medical care more quickly.
You may want to ask your eye care specialist or healthcare provider the following:
A blocked tear duct can be unpleasant and painful for adults. And if a child you care for has one, it’s understandable to feel worried or anxious. Fortunately, blocked tear ducts are extremely treatable. Most children recover quickly, especially with simple face massage techniques. The outlook is usually positive for adults, too, especially with certain causes or contributing factors.
If you think your child has (or you have) a blocked tear duct, talk to an eye care specialist or healthcare provider. Timely diagnosis and care can make a big difference in helping wipe away backed-up tears and the worries that come with them.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic Children’s provides expert diagnosis and treatment for children with a blocked tear duct.
