Legg-Calve-Perthes disease affects the growing end of the femur bone that fits into your child’s hip socket. It causes the end of the bone to break down and then regenerate over several years. This process can alter the shape of the bone and how it fits in the socket. Your healthcare provider will work to prevent or correct this deformity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
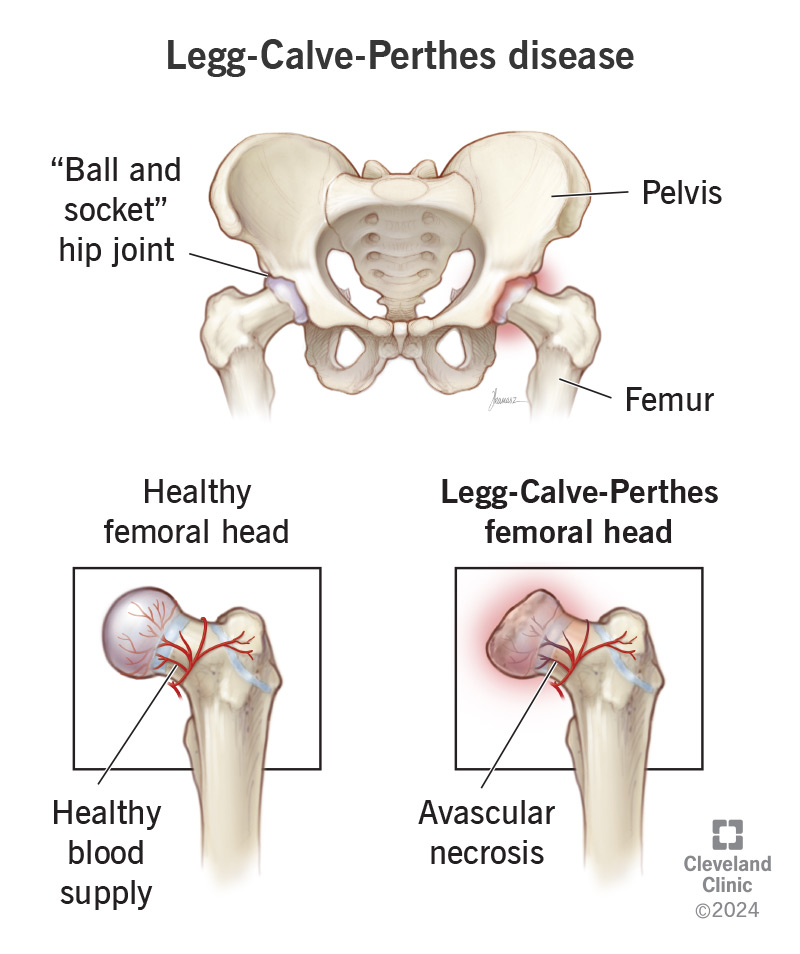
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/legg-calve-perthes-disease)
Legg-Calve-Perthes disease (also known as Perthes disease) is a rare condition that affects children’s hips. It starts when the top of the thigh bone (femur) temporarily loses its blood supply.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Because the bone needs fresh blood to get oxygen and nutrients, it starts to die and break down. After the blood flow returns to normal, your child’s bone will slowly repair itself. But it may not have its original shape and size.
Perthes disease is most common in kids ages 5 to 7. But it can affect kids as young as 2 or as old as 12. It progresses in stages. First, your child’s affected bone breaks down from a loss of blood supply. Then, after blood flow is restored, it will start to regrow. The breakdown phase may take up to a year. The rebuilding phase may last two to five years.
How much it affects your child depends on how much their thigh bone changes. Some kids lose more bone tissue than others. This can happen for a few reasons:
Treatments can help your child’s femur regrow correctly. Most children have no long-term complications after treatment. Kids who continue to have poorly fitted hip joints will have ongoing symptoms. Hip dysplasia can lead to complications like arthritis later in life.
Signs and symptoms of Perthes disease develop over time. You or your child might start to wonder what’s up when symptoms appear and don’t seem to ever get better.
Advertisement
Early symptoms might include:
Later signs and symptoms of LCPD may include:
Perthes disease happens when something slows or stops the blood supply to the head of your child’s femur. Healthcare providers aren’t always able to find a specific cause.
Blood flow can stop if a blood vessel is blocked or squeezed. Artery disease or a blood clot might block it from the inside.
Swelling might compress a blood vessel from the outside. Sudden trauma or a repetitive strain injury can cause swelling in your child’s hip. This can cut off blood flow to their thigh bone.
1 in 10 cases appear genetic. It’s possible that certain genetic changes can pass through generations in your biological family. Experts have identified that a change in the COL2A1 gene may cause LCPD.
Perthes disease is five times more common in males. About half of kids who develop it have some type of blood-clotting disorder.
Your child may have a higher risk of developing Legg-Calve-Perthes if they have:
Environmental factors can also play a role. These are things about where you live or spend time that can affect your health. Your child’s risk of LCPD can increase if they:
A healthcare provider will begin with a thorough physical examination. They’ll use X-rays to take pictures of your child’s bones. X-rays can show evidence of Perthes syndrome. They’ll also show its stage and severity. In some cases, your child might need an MRI to see certain features in more detail.
Advertisement
Treatment for Legg-Calve-Perthes depends on a few factors, including:
In general, younger kids tend to do better with more conservative treatments. That’s because their bones naturally grow and develop faster. Older children might need more help to restore their bone tissue.
Your child’s healthcare team will develop a personalized treatment plan. This may include:
Advertisement
It can take your child several years to recover completely from Legg-Calve-Perthes disease. This can intrude on their childhood, to some extent. But when it’s over, they should be able to return to their usual activities.
Perthes syndrome is temporary, but it can cause permanent changes. Kids who don’t get the right treatment soon enough have an increased risk of hip osteoarthritis later in life. But most children don’t have long-term complications.
Legg-Calve-Perthes disease is an unexpected diagnosis. You might have a lot of questions. Your healthcare provider can help (and your child) understand what’s going on. Don’t be afraid to ask any questions you have. Encourage your child to ask questions, too.
There are lots of reasons for optimism. Most kids don’t have too much discomfort during treatment. They might have some limitations, but they’re usually temporary. Your child will need some type of orthopedic therapy. But in the end, most kids have no long-lasting symptoms or issues.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
As your child grows, you need healthcare providers by your side to guide you through each step. Cleveland Clinic Children’s is there with care you can trust.
