Oppositional defiant disorder (ODD) is a condition in which your child displays a pattern of uncooperative, defiant and angry behavior toward people in authority. ODD is treatable with psychotherapy and parent management training.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
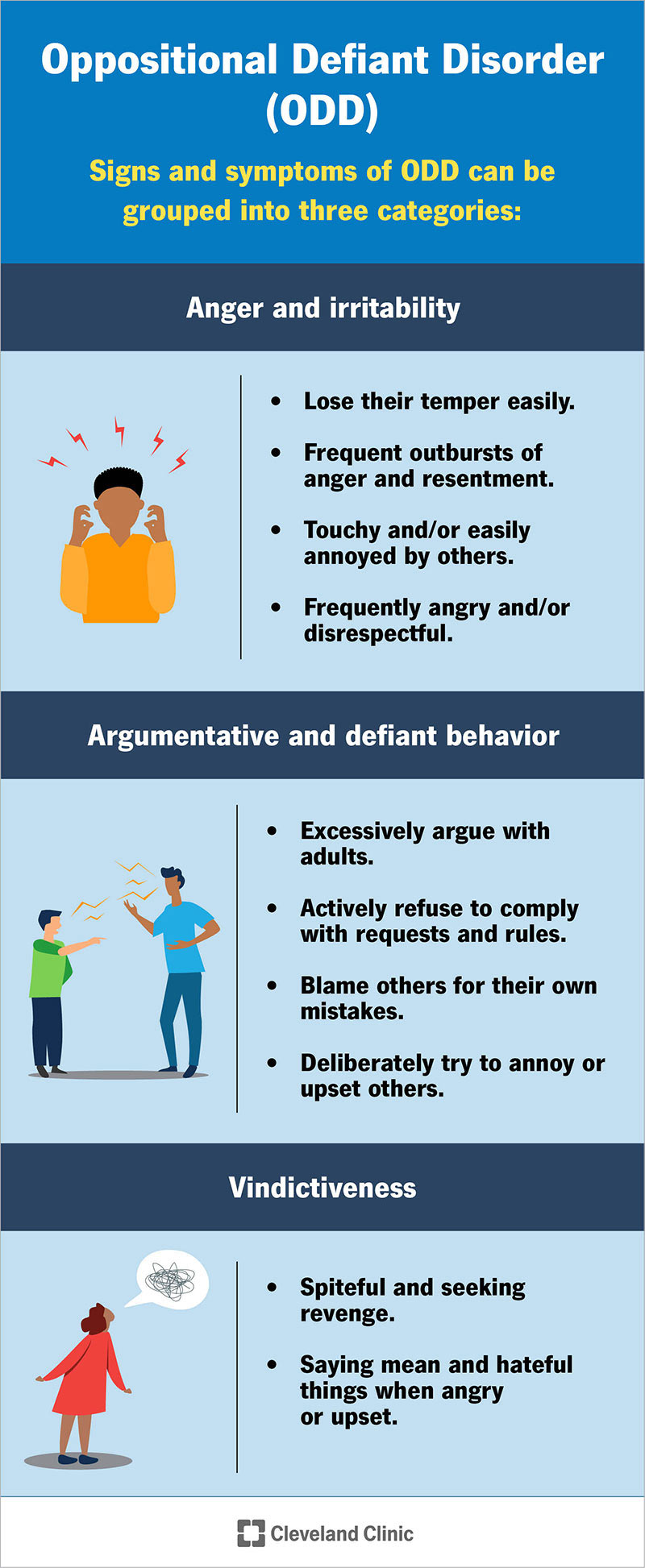
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9905-oppositional-defiant-disorder)
Oppositional defiant disorder (ODD) is a behavior condition in which your child displays a continuing pattern of uncooperative, defiant and sometimes hostile behavior toward people in authority. This behavior often disrupts your child’s normal daily functioning, including relationships and activities within their family and at school.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s common for children — especially those two to three years old and in their early teens — to be oppositional or defiant of authority once in a while. They might express their defiance by arguing, disobeying or talking back to adults, including their parents or teachers. When this behavior lasts longer than six months and goes beyond what’s usual for your child’s age, it might suggest that they have ODD.
The majority of children and teens who have ODD also have at least one other mental health condition, including:
About 30% of children with ODD develop a more serious behavior condition called conduct disorder. ODD behaviors can continue into adulthood if ODD isn’t properly diagnosed and treated.
Conduct disorder (CD) is a condition in which your child or adolescent shows an ongoing pattern of aggression toward others. They also show serious violations of rules and social norms at home, in school and with peers.
These rule violations may involve breaking the law. Children with CD are more likely to get injured and may have difficulties getting along with peers.
Advertisement
Signs of conduct disorder include:
Approximately 40% of children with attention-deficit/hyperactivity disorder (ADHD) also have oppositional defiant disorder or a related conduct disorder. While these two conditions commonly occur together, they’re distinct conditions.
ODD is related to a child’s conduct and how they interact with their parents, siblings, teachers and friends. ADHD is a neurodevelopmental disorder that causes a person to be easily distracted, disorganized and excessively restless.
ODD most commonly affects children and teenagers, but it can also affect adults. It most commonly begins by age 8.
Some children outgrow ODD or receive proper treatment for it, while others continue to have symptoms through adulthood.
Boys are more likely to have ODD in their younger years than girls. But teenagers are affected equally.
Your child is more likely to develop ODD if they have the following risk factors:
Researchers estimate that oppositional defiant disorder affects 2% to 11% of children. This range is so wide because some children may be misdiagnosed as having conduct disorder, and teenagers, as a population, are often underdiagnosed.
The prevalence of ODD declines with increasing age.
Signs and symptoms of oppositional defiant disorder usually begin by age 8. Symptoms usually remain stable between the ages of 5 and 10 and typically, but not always, decline afterward.
The symptoms are often apparent in multiple settings but may be more noticeable at home or school.
Signs and symptoms of ODD can be grouped into three categories:
In addition, many children with ODD are moody, easily frustrated and have low self-esteem. They also might misuse drugs and alcohol.
Advertisement
Signs of anger and irritability are part of the diagnosis of ODD. If your child has ODD, they may:
Argumentative and defiant behavior is part of the diagnosis of ODD. If your child has ODD, they may:
Signs of vindictiveness in ODD include:
Researchers believe that the cause of oppositional defiant disorder is a complex combination of biological, genetic and environmental factors:
Advertisement
Mental health professionals diagnose oppositional defiant disorder (ODD) if your child meets four or more of the symptom criteria as described in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) for at least six months. The DSM-5, published by the American Psychiatric Association, is the standard reference book for recognized mental illnesses. The symptoms must also be severe and disruptive to daily life.
Your child will likely need to see a child and adolescent psychologist or psychiatrist if they’re showing signs of ODD. These mental health professionals use specially designed interview and assessment tools to evaluate your child for a mental health condition.
Psychiatrists and psychologists often rely on reports from the child’s parents, siblings, friends and teachers to get a full understanding of their behavior.
Your child’s psychologist or psychiatrist will carefully assess your child. They must distinguish oppositional defiant disorder from the following conditions, which may cause similar symptoms:
Advertisement
Treatment for ODD varies based on many factors, including:
Treatment of ODD should involve your child, your family and their school.
Treatment usually consists of a combination of the following:
Parent management therapy (PMT) is the main treatment for oppositional behaviors. It teaches parents ways to change their child’s behavior in the home by using positive reinforcement to decrease unwanted behaviors and promote healthy behaviors.
There are different types of training programs, which usually involve multiple sessions over several weeks. During the sessions, parents learn to identify problem behaviors, as well as positive interactions, and to apply punishment or reinforcement as appropriate.
PMT has been shown to decrease conduct problems in multiple contexts and family backgrounds significantly.
Psychotherapy (talk therapy) is a term for a variety of treatment techniques that aim to help you identify and change troubling emotions, thoughts and behaviors. Working with a mental health professional, such as a psychologist or psychiatrist, can provide support, education and guidance to your child and your family.
Common types of psychotherapy that help treat ODD include:
Supportive interventions to improve school performance, peer relationships and problem-solving skills are very useful in the treatment of ODD.
These interventions may include:
Although there isn’t medication formally approved to treat ODD, your child’s healthcare provider or psychiatrist might prescribe certain medications to treat other conditions they may have, such as ADHD, OCD or depression. If left untreated, these conditions can make the symptoms of ODD worse.
Children with ODD can experience significant issues in school, at home and in social relationships.
Mild to moderate forms of ODD often improve with age, but more severe forms can evolve into conduct disorder.
A lack of treatment and parental support often leads to a poor prognosis for oppositional defiant disorder, while adequate treatment of coexisting conditions (such as ADHD or OCD), individual and/or family therapy, and positive parenting are associated with a good prognosis.
Although it might not be possible to prevent oppositional defiant disorder, recognizing and acting on symptoms when they first appear can minimize distress to your child and family. It can also help prevent many of the problems associated with the disorder. Family members can learn steps to take if signs and symptoms return, as well.
In addition, providing a nurturing, supportive and consistent home environment might help reduce symptoms and prevent episodes of defiant behavior.
If your child has oppositional defiant disorder, aside from getting them professional care, you can help them and yourself in the following ways:
If your child has been diagnosed with oppositional defiant disorder, and their behavior becomes more severe or disrupts family or school life, talk to their mental health provider.
If your child displays behavior that harms or endangers others, such as other children or animals, it’s important to find them immediate care.
Children and teens who are defiant or very disruptive can be very challenging for parents. While it’s normal for young children and teens to show defiant behavior from time to time, frequent and disruptive behavior may indicate oppositional defiant disorder (ODD).
Starting treatment early for ODD is important, and the first step to treatment is to talk with a healthcare provider or a mental health provider. Don’t be afraid to ask your healthcare provider questions. They’re available to help.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Your mental well-being is just as important as your physical well-being. Cleveland Clinic’s mental health experts can help you live life to the fullest.
