Deep vein thrombosis is a blood clot in a vein located deep within your body, usually in your leg. It can pose serious health risks. Symptoms include pain, swelling, redness and warmth in your leg. You take some treatments, like medicines, for months, while you may wear compression stockings for two years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
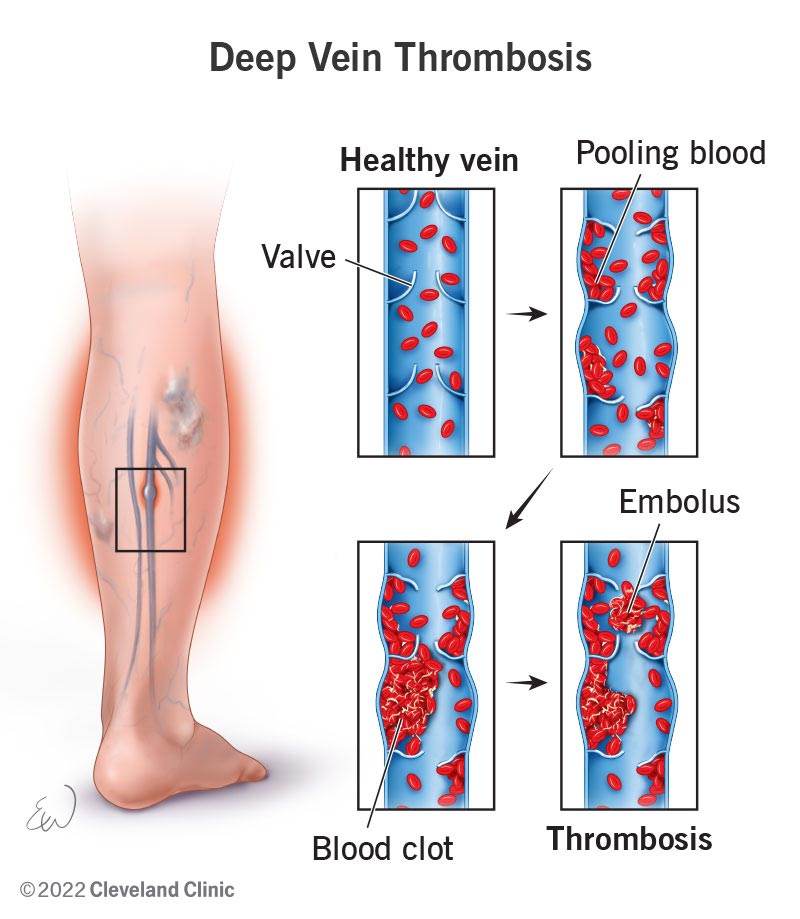
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16911-deep-vein-thrombosis)
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) develops in a vein deep in your body, often in your leg. This can happen because of a vein injury or slow-flowing blood. The blood clot may partially or completely block blood flow through your vein.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most DVTs happen in your calf, thigh or pelvis. But they also can occur in other parts of your body, including your arm, brain, intestines, liver or kidney.
Deep vein thrombosis (also called venous thrombosis) is common. You need quick diagnosis and treatment to prevent life-threatening complications.
A DVT usually forms in the veins of your legs or arms. Some people have mild symptoms or none at all. DVT symptoms include:
Some people don’t know they have a DVT until the clot moves from a leg or arm and travels to a lung. This is a pulmonary embolism (PE). Symptoms of this include chest pain, shortness of breath, cough with blood, lightheadedness and fainting.
It’s important to call your provider right away or go to the emergency room if you have deep vein thrombosis or PE symptoms. Don’t wait to see if your symptoms go away. Get treatment right away to prevent serious complications.
Advertisement
Slow blood flow in a damaged deep vein after being inactive for a long time can cause deep vein thrombosis. This often comes after an injury, surgery or hospital stay. This is because you’re lying in bed most of the time instead of moving like you normally would. It’s also because there’s a high amount of inflammation in your body and blood vessels.
A DVT can also happen when you’re not moving for more than four hours because of travel. You may be sitting for a long time in a car, truck, bus, train or airplane.
Some people have a personal or family history of DVT or a blood-clotting disorder that increases the risk of blood clots. Others may have these risk factors for deep vein thrombosis:
Without prompt treatment, a DVT may lead to serious complications like:
Your healthcare provider will do a physical exam and review your medical history. You’ll also need to have blood tests or imaging tests. These include:
DVT treatment aims to keep the clot from getting bigger or breaking off and lessen the risk of another blood clot. Deep vein thrombosis treatment includes medications, compression stockings and elevating your affected leg(s) at different times throughout the day. In rare cases, you may need invasive treatments.
Advertisement
Treatments include:
Tell your healthcare provider if your symptoms aren’t getting better. You should also tell them if you’re bruising too easily or having heavy periods. You should get emergency care if the blood thinners you’re taking make you bleed too much, or cause problems like bright red blood in vomit or poop.
Advertisement
You should have follow-up appointments while you wait for the blood clot to break up. These visits may include blood tests and ultrasounds.
Questions to ask your provider may include:
A DVT can take several months or even over a year to come apart. You’ll need to continue with treatments until your provider tells you to stop. You may need blood tests to make sure you’re getting the right dose of blood thinners. Your provider may want to do more ultrasounds later to see whether your blood clot is still in the same place, improving or getting larger.
A deep vein thrombosis may make it harder for you to use your legs at first because of leg pain and swelling. But you’ll be able to slowly return to your normal activities.
If your legs feel swollen or heavy, lie in bed with your heels propped up about 5 to 6 inches. This helps improve circulation and decreases swelling. Wearing knee-high compression stockings can help, too. These can reduce your leg pain and swelling by at least half if you wear them daily.
You can prevent deep vein thrombosis from happening (or repeating) in these ways:
Advertisement
Make lifestyle changes, like eating nutritious foods, being active and avoiding tobacco products.
If you have a deep vein thrombosis, you’re not alone. They’re common, but prompt treatment is important with this condition. Several treatments can help. Your healthcare provider can customize your care to your situation. If they prescribe blood thinners, be sure to keep up with all your follow-up visits so you know you’re getting the correct dose.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
