Degenerative disk disease occurs when the cushioning in your spine begins to wear away. After age 40, most people experience some spinal degeneration. But the condition doesn’t always cause symptoms. When it does, neck and back pain can be intense. The right treatment can lead to pain relief and increased mobility.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
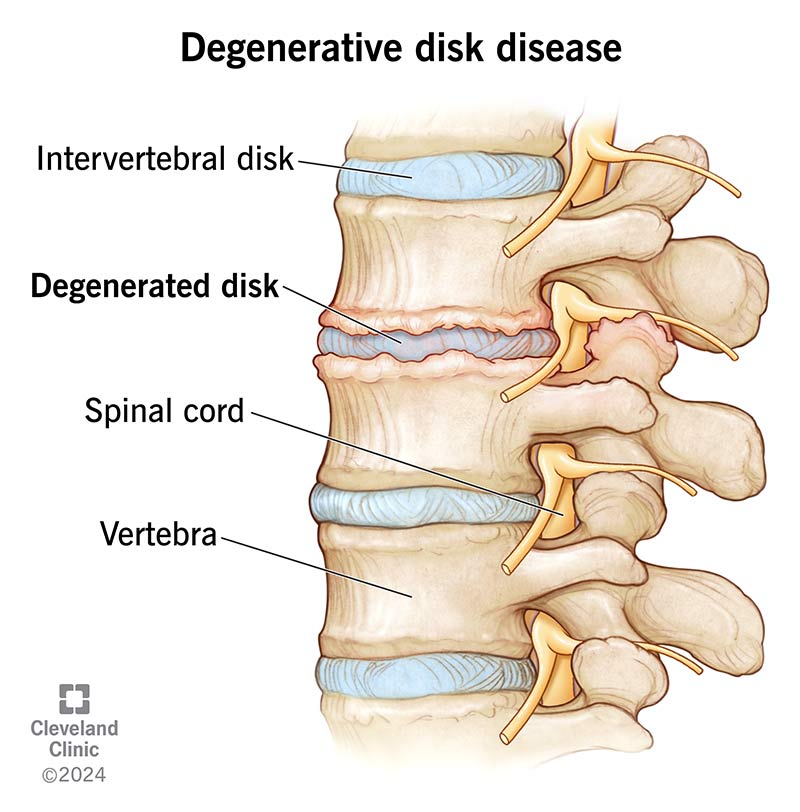
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/degenerative-disk-disease)
Degenerative disk disease (sometimes spelled degenerative disc disease) isn’t actually a disease, but rather, it’s a condition that occurs when your spinal disks wear down. Spinal disks are rubbery cushions between your vertebrae (bones in your spinal column). They act as shock absorbers and help you move, bend and twist comfortably. Everyone’s spinal disks degenerate over time — it’s a natural part of aging.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When the cushions wear away, the bones can start to rub together. This contact can cause pain and other problems, like:
Disk degeneration mostly affects your lower back (lumbar spine) or neck (cervical spine).
Advertisement
Almost everyone has some disk degeneration after age 40, even if they don’t develop symptoms. It can lead to back pain in about 5% of adults.
The most common degenerative disk disease (degenerative disc disease) symptoms are neck pain and back pain. You may experience pain that:
Degenerative disk pain:
Spinal disks wear down as a natural part of aging. Especially after age 40, most people experience some disk degeneration. But not everyone experiences pain.
You might have pain if your spinal disks:
Degenerative disk disease is most common in people age 40 and older. Some factors increase your risk of developing degenerative disk disease, including:
Degenerated disks can increase your risk of developing other spinal conditions. Common spine problems include:
To diagnose degenerative disk disease (degenerative disc disease), your healthcare provider may start by asking you about your symptoms. Questions may include:
Your healthcare provider may use imaging scans, like X-ray, CT or MRI to help with the diagnosis of degenerative disk disease. These tests can show your healthcare provider the state and alignment of your disks. Your provider may also conduct a physical exam to check your:
Advertisement
Healthcare providers use the following four stages when diagnosing degenerative disk disease:
Usually, your healthcare provider will recommend noninvasive degenerative disk disease treatment options first. Your treatment may include:
Advertisement
Some people find pain relief through at-home remedies. At-home treatments may decrease pain for a short time. But they’re not a long-term treatment for severely degenerated disks. You may try:
Most people don’t need surgery for degenerative disk disease. But if you’ve tried multiple nonsurgical treatments and have persistent pain and/or weakness, surgery may be a good option.
Your surgeon may use one of a few types of spinal decompression surgery:
Advertisement
Most people who have surgery for degenerative disk disease experience long-term pain relief. But even after surgery, you need to continue exercising and stretching to keep your back strong and healthy.
Many people use nonsurgical and at-home treatments to manage pain long term. If you have mild to moderate back pain, you’ll need to continue treatment to keep the pain at bay.
You can prevent or slow the progression of spinal degeneration through lifestyle changes. Some of these include:
Things to avoid with degenerative disk disease include:
You may want to ask your healthcare provider:
Degenerative disk disease (degenerative disc disease) occurs when your spinal disks break down. Unfortunately, it’s just a natural part of aging. When these disks wear out, you’ll typically experience back pain and stiffness. For some people, home remedies like hot and cold therapy can decrease pain. When the pain is severe, you may benefit from spinal injections or spine surgery. A spine specialist can help you determine which treatment is best for you.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Back pain can stop you in your tracks. But you don’t have to live like that. Cleveland Clinic is here to help you get moving again.
