What is ventricular tachycardia?
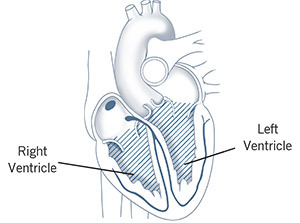
The ventricles are the heart’s two lower chambers. Blood flows from the top chambers of the heart (atria) into the ventricles, then it moves to the lungs and through the aorta to be circulated throughout the body. Tachycardia is a heart rate higher than 100 beats per minute. A normal resting heart rate is 60 to 100 beats per minute. Ventricular tachycardia starts in the heart’s lower chambers. Most patients who have ventricular tachycardia have a heart rate that is 170 beats per minute or more.
What causes ventricular tachycardia?
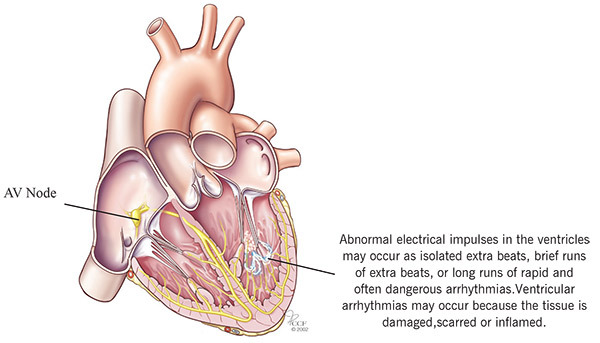
Your heart rate is controlled by electrical signals that move across the heart muscle. When something goes wrong and signals are sent too quickly, it can cause tachycardia.
Most patients with ventricular tachycardia have another heart problem, such as coronary artery disease, high blood pressure, an enlarged heart (cardiomyopathy) or heart valve disease. The condition can also develop after a heart attack (myocardial infarction) or heart surgery because of scar tissue that forms on the heart.
Other, non-heart-related causes of ventricular tachycardia include some medications, an imbalance in electrolytes (the minerals that control heart rhythm), too much caffeine or alcohol, recreational drugs, exercise and certain genetically transmitted conditions. Sometimes the cause is unknown.
You are also more likely to have ventricular tachycardia as you get older or if you have a family history of heart rhythm disorders.
What are the symptoms of ventricular tachycardia?
During an episode of ventricular tachycardia, the heart is beating so fast that the blood pressure drops so the heart cannot pump enough oxygen to every part of the body, and this is what causes symptoms. Although some people with ventricular tachycardia do not experience any symptoms, the most common symptoms are dizziness, lightheadedness, palpitations, shortness of breath or chest pain. When the heart rate is extremely high or the ventricular tachycardia persists for more than a few seconds, it can cause fainting, unconsciousness or cardiac arrest and death.
If you experience unexplained fainting, dizziness, lightheadedness, shortness of breath or palpitations, you should be evaluated for possible ventricular tachycardia. Chest pain, difficulty breathing and a rapid pulse are urgent symptoms of a potentially fatal ventricular tachycardia, and you must seek emergency help immediately to avoid the risk of cardiac arrest and death.
How is ventricular tachycardia diagnosed?
Your doctor will talk to you about your symptoms and medical history. You will also have testing to determine if you have ventricular tachycardia.
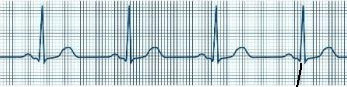
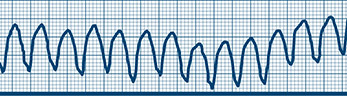
The most common test used to diagnose ventricular tachycardia is an electrocardiogram (ECG/EKG). An EKG records your heart’s electrical activity. Electrodes (small sticky patches) are placed on your chest and arms to record the heart’s rhythm, and the pattern prints on graph paper. Your doctor may also want to track your heart rhythm at home. If so, you will wear a Holter monitor at home for 24 to 48 hours.
Your doctor may refer you to a specialist to electrophysiology testing. During the test, catheters (long, thin tubes) with electrodes are inserted through the veins at the groin and placed directly in the heart. The electrical activity in different parts of the heart is recorded so your doctor can create a map of the heart’s electrical impulses and see where the electrical problem starts.
Normal Heart Rhythm recorded on EKG
Ventricular Tachycardia recorded on EKG
What treatments are available?
Treatment for ventricular tachycardia involves managing any disease that causes the condition. These treatments may improve or prevent the abnormal heart rhythm from returning.
In emergency situations, CPR, electrical defibrillation and IV medications may be needed to slow the heart rate.
Nonemergency treatment usually includes radiofrequency catheter ablation (RCA) or an implantable cardioverter defibrillator (ICD).
Radiofrequency Catheter Ablation
Radiofrequency catheter ablation is a procedure performed by a cardiac electrophysiologist, which is a cardiologist who specializes in treating patients with heart rhythm disorders. In the first part of the procedure, the doctor uses electrophysiology techniques to pinpoint the location in the heart where the abnormal rhythm begins.
In the second step, the doctor uses a catheter with a special tip that emits a high-frequency form of electrical current. The current is used to destroy a tiny amount of tissue in the area of the ventricle where the abnormal rhythm begins. This is called an ablation procedure.
Ablation of ventricular tachycardia has a long history of safety and success. For some patients, ablation completely cures the abnormal rhythm, and no other treatment is needed. Ablation can also improve treatment with an implantable cardioverter defibrillator (ICD).
Implantable Cardioverter Defibrillator (ICD)
An ICD is a device that is implanted under the skin. It monitors and controls the heart’s rhythm. If it detects an episode of ventricular tachycardia, it acts quickly to get your heart back to a normal rhythm. An ICD consists of a pulse generator, which is about the size of a pager, and one or more lead wires that connect the pulse generator to the heart. The leads are inserted through the veins and positioned in the heart. The leads send information about the heart’s electrical activity to a computer microchip in the pulse generator. If the computer detects an abnormal heartbeat, the pulse generator sends an electrical signal across the lead(s) to the heart to restore a normal heart rhythm.
Clinical studies show that ICDs can stop life-threatening ventricular tachycardias in nearly all patients.
Medications
Medications to slow the heart rate are another treatment option for patients with ventricular tachycardia. These drugs can be effective but are associated with some serious, potentially fatal side effects, and they are not used as much as they were in the past.
Follow-up Care
It is important to keep your appointments for regular follow-up visits. Your doctor will want to see how you’re doing, make sure your treatment is working and talk about any symptoms or changes you’ve had. You should also follow a heart-healthy diet and exercise plan that your healthcare team recommends for you.