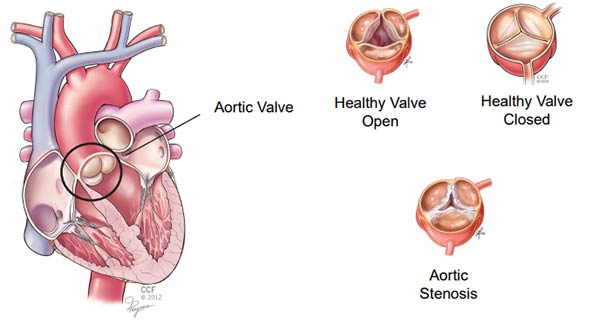
What is transcatheter valve replacement?
Transcatheter aortic valve replacement (TAVR) is a treatment option for some patients with severe aortic stenosis.
Who can have TAVR?
A thorough evaluation by a multidisciplinary team is needed to find out if you are a candidate for TAVR. The evaluation takes several days and includes a review of your health history, exams, tests and meeting with multiple members of the TAVR team. The team reviews the information within 4 to 6 weeks of the evaluation to make a decision. If you are not a candidate for TAVR, we will talk to you about other treatment options.
Preparing for the procedure
If you are scheduled for TAVR at Cleveland Clinic, you will have an appointment before the procedure. You will meet members of your TAVR team and get detailed information about what to expect before, during and after the procedure. Your doctor will also talk to you about the risks and benefits of TAVR. Please write down questions and concerns you have and share them with your team during this appointment.
How long does the procedure take?
The TAVR procedure takes about 2 hours. This includes time to get you ready (prep), the procedure (about an hour) and time to take you to and from the operating room.
Will I be asleep?
You will either get general anesthesia (“be asleep”) or conscious sedation (“twilight sleep”). The type of anesthesia you get depends on how the valve is put in place.
What is a pacing wire?
A pacing wire is a wire attached to your heart so your doctor can adjust your heart rate during the procedure. The wire may stay in place for a day or so after the procedure, if needed.
How is the valve put in place?
The new aortic valve is put in place with a long, thin tube called a catheter. The catheter goes through a small incision into a blood vessel. The doctor uses an X-ray and dye (fluoroscopy) to see the valve as it moves through the blood vessel to your heart. The new valve is secured inside the diseased valve.
There are several ways to put the valve in place. Your doctor may use one of these approaches or talk to you about other options:
Transfemoral Approach
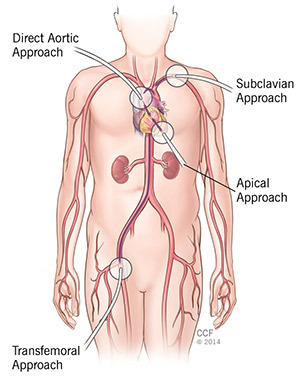
- Small incision in your groin.
- Catheter goes into your femoral artery.
- Conscious sedation.
Transapical Approach
- 4-inch incision between your ribs.
- Catheter goes through the tip of your heart.
- General anesthesia.
Direct Aortic Approach
- J-shaped incision at the top of your breastbone (sternum).
- Catheter goes into your aorta.
- General anesthesia (you are “asleep”).
Subclavian Approach
- Small incision near your shoulder.
- Catheter goes into your subclavian artery.
- General anesthesia or conscious sedation.
Your doctor will test the valve after it is in place. Then, the catheter is removed and your incision is closed.
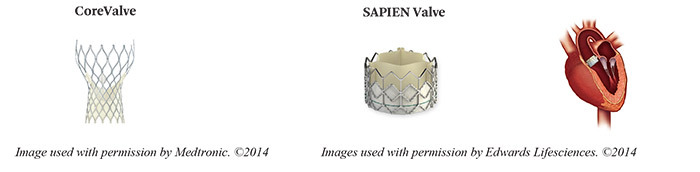
What type of valve will I get?
Your aortic valve will be replaced with a valve made from animal tissue (biological). The tissue is supported with a metal frame. Despite the metal frame, you will not need to take blood thinners (unless you already take one for another reason).
Most patients who have TAVR at Cleveland Clinic get a CoreValve (Medtronic) or SAPIEN valve (Edwards). Your doctor may talk to you about using a different type of valve, based on your needs.
How long will the new valve last?
Your new valve is designed to work like a healthy natural valve. It can last 10-15 years, but this can vary from patient to patient. You will have an echo at each follow-up visit to check the valve for problems.
How will I feel after the procedure?
You will have some pain/discomfort at the incision site(s). It is important to tell your nurse how you feel so we can manage your pain as soon as possible. You may still have the symptoms you had before TAVR. These should clear up within a short time. Most patients feel better and have a better quality of life within 30 days of the procedure and continue to feel better after that.
When can I go home?
You will most likely be able to go home the same day. But, depending on the approach that was used, you may need a longer recovery that includes time in the hospital. Your doctor will talk to you about what to expect before your TAVR.
When do I see my doctor for follow-up care?
You will have several follow-up visits with your cardiologist:
- One week after the procedure.
- Within one month of the procedure - visit and echocardiogram (echo).
- Six months after the procedure.
- One year after the procedure. Your cardiologist may want to see you sooner.
It is very important to keep all of these appointments, even if you feel fine.
What restrictions will I have after the procedure?
You will need to limit some activity and will not be able to drive until your doctor tells you it is okay to do so. Please see the Important Information to Follow When You Get Home (below) for more information. You will also get details discharge instructions before you leave the hospital.
Do I need to take medicine after the procedure?
Please make sure you ask your doctor about the types and amounts of medicine you need to take after TAVR. Share any questions or concerns you have.
- You may need to take different types or amounts of medicine after TAVR.
- You may not need to take some of the medicine you took before TAVR.
- If you have diabetes, ask your doctor if you need to make changes after your procedure.
- Blood thinners: You will need to take an 81-mg aspirin (“baby” aspirin) every day. You may also need to take Plavix (clopidogrel) for 30 days after your procedure. These are in addition to any blood thinners you may already take. Please tell your cardiologist if you cannot take these medications or if you have recently had problems with bleeding.
- You will need to take an antibiotic before you have certain dental and medical procedures. Having a replacement valve increases your risk of a potentially deadly heart infection called endocarditis. Talk to your doctor before you have any procedure to find out if you need to take an antibiotic to reduce this risk.
Can I have Magnetic Resonance Imaging (MRI) after the procedure?
You will get an ID card with information about your valve. Please carry this card with you at all times and show it to your doctor, nurse or radiology technician before you have an MRI.
Do I need to make lifestyle changes?
It is important to follow your plan of care, which includes living a heart-healthy lifestyle. This will help you have the best results possible after your TAVR procedure. Your healthcare team can help you set and meet your goals. It is up to you to commit to those goals that include taking your medicine as prescribed, eating a heart-healthy diet, not using tobacco or nicotine products, getting regular exercise and keeping your follow-up appointments.
Will insurance pay for TAVR?
Our financial team will work with your insurance carrier to get pre-authorization for the tests you need before your TAVR procedure and the procedure itself. We will let you know before you go to any appointments if there are any problems with your insurance coverage.
Information To Follow When You Get Home
If your TAVR was done with a transfemoral (groin) approach:
- Do not strain during bowel movements for 3 to 4 days after the procedure. This helps prevent bleeding from the incision area.
- Do not lift anything that weighs more than 10 pounds or push/pull heavy objects for the first 5 to 7 days after the procedure.
- Do not do anything strenuous for 5 days after the procedure. This includes most sports, such as jogging, golfing, playing tennis and bowling.
- Walk up and down the stairs more slowly than usual.
- Gradually increase your activity level during the week after the procedure. You should be back to your normal routine after the first week.
- Do not have sexual intercourse. Ask your doctor when it is safe to resume sexual activity.
- Do not drive until you get the OK from your doctor.
- Join a Stage II cardiac rehab program after you talk to your doctor at your first follow-up visit.
Take care of your incision
- You will have a bandage over the incision. You can remove it the morning after your procedure. It is easiest to remove by wetting the tape first while showering.
- Wash your hands before you touch your incision site.
- Place an adhesive bandage over the area. It is normal for the wound site to be black and blue for a couple of days. The area may also be pink and swollen, and there may be a small lump (about the size of a quarter).
- Wash the site at least once a day with soap and water. Do not use perfumed soap or shower gel. Put soap on your hand or a washcloth and gently cleanse and rinse the area. Do not rub the area.
- Keep the area clean and dry, except when showering.
- Do not rub cream, lotion or ointment on the incision area.
- Do not soak in water / take a bath or swim until the incision is completely healed.
- Wear loose-fitting clothing over the incision area.
If your TAVR was NOT done using a transfemoral (groin) approach:
- Do not lift anything that weighs more than 10 pounds for 8 weeks after your procedure.
- Do not drive until you get the OK from your doctor.
- Walk every day, and continue to increase your effort and length of time you walk.
- Do not do anything strenuous until you get the OK from your doctor.
- Do not have sexual intercourse. Ask your doctor when it is safe to resume sexual activity.
- Join a Stage II cardiac rehab program after you talk to your doctor at your first follow-up visit.
- If your TAVR was done using a direct aortic approach, it It will take about 8 weeks for your sternum to completely heal.
Take care of your incision
- Wash your hands before you touch your incision.
- Wash the site at least once a day with soap and water. Do not use perfumed soap or shower gel. Put soap on your hand or a washcloth and gently cleanse and rinse the area. Do not rub the area.
- Keep the area clean and dry, except when showering.
- Do not rub cream, lotion or ointment on the incision area.
- Do not soak in water / take a bath or swim until the incision is completely healed.
When to Call 911
Call 911 or get a ride to your local emergency department if you have:
- Chest pain or discomfort that lasts 5 minutes and does not go away after you rest or take medication. The pain may go away and come back again. It may feel like indigestion or heartburn, like there is weight/pressure/squeezing in your chest, or your chest may ache, burn, feel numb or full. If you have a prescription for nitroglycerin, put a tablet / single spray under your tongue and wait 5 minutes. If the pain continues, call 911. If you have chronic stable angina and have symptoms after you take nitro and wait 5 minutes, take another tablet. You can take up to 3 tablets (1 every 5 minutes, for 15 minutes). If you still have angina after 15 minutes, call 911.
- Uncontrolled bleeding from the incision area. Bleeding is rare. But if it happens, take off the bandage. Put clean gauze or a washcloth over the incision and put pressure on the area. Call 911 if the bleeding doesn’t stop after 20 minutes.
- Fast heart rate - more than 120 beats per minute, especially if you are short of breath.
- New irregular heartbeat.
- Trouble breathing or shortness of breath that does NOT stop when you rest.
- Sudden numbness or weakness in your arms or legs.
- Fainting.
- Pain or discomfort in your arm(s), left shoulder, back, neck, jaw or stomach.
- Sweating or a “cold sweat.”
- Feeling full - This can feel like indigestion or heartburn. You may feel like you’re choking.
- Nausea or vomiting.
- Feeling light-headed, dizzy, very weak or anxious.
When to Call Cleveland Clinic
Call your doctor or other contact number you receive if:
- The incision area is red, unusually warm, or if there is pus-like drainage.
- You have a groin incision and your leg is cold, numb, tingling, discolored or very swollen.
- You have a groin incision and there is a golf ball-sized lump in the area.
- You have extreme pain or swelling in the incision area.
- You have a temperature higher than 101 degrees F.
- You have questions about your procedure, medications, follow-up schedule or plan of care.