What is syncope?
Syncope (pronounced "sin ko pea") is the medical term for fainting/passing out.
What causes syncope?
Syncope is caused by a temporary drop in the amount of blood that flows to your brain. Many patients who have syncope have a medical condition that causes the condition.
What are the symptoms of syncope?
Many times, you can feel an episode of syncope coming on. Premonitory symptoms are feelings that happen before you pass out. They include feeling:
- Lightheaded.
- Nauseous.
- Dizzy.
- Drowsy or groggy.
- Unsteady or weak when standing.
- Clammy.
- Shaky.
You may also have a headache, changes in your vision (seeing spots, tunnel vision) or heart palpitations (irregular heartbeats that feel like fluttering in your chest).
If you have these symptoms, you will likely be able to stop yourself from passing out by sitting or lying down and putting your legs up.
If you do pass out, you will likely become conscious and alert right away, but you may feel confused for a bit.
Types of Syncope
There are three main types of syncope — reflex syncope, orthostatic syncope and cardiac syncope. The type you have depends on what causes the problem.
Reflex syncope
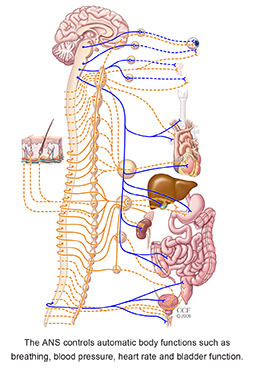
Reflex syncope happens when certain situations trigger a change in the way your body circulates blood. When you stand up, gravity causes blood to settle in the lower part of your body, below your diaphragm. When that happens, the heart and autonomic nervous system (ANS) work to keep your blood pressure stable. If you have reflex syncope, the ANS can’t keep the pressure stable, and it drops, causing you to faint.
Vasovagal syncope is the most common type of reflex syncope. It is caused by emotional stress, suchas pain, fear and anxiety. This type of syncope is most common in young people.
Situational syncope is another type of reflex syncope. Common triggers for this type are:
- Coughing or sneezing.
- Gastrointestinal functions, such as swallowing and bowel movements.
- Eating.
- Exercising and weightlifting.
- Urinating.
- Playing a brass or wind instrument.
Carotid sinus syncope is a type of reflex syncope that can happen when you turn your neck or wear a tight collar.
About one-third of patients with reflex syncope have unknown causes/triggers.
Orthostatic syncope
Orthostatic hypotension (postural syncope/ postural hypotension) means the blood vessels can’t get smaller (constrict) like they should when you stand up. This causes blood to collect in your legs, and your blood pressure quickly drops, causing you to faint.
Orthostatic hypotension is related to:
- Primary autonomic failure. This means there is a condition such as Parkinson’s disease or multiple system atrophy that keeps the ANS from working like it should.
- Secondary autonomic failure. This means a condition such as diabetes, amyloidosis or a spinal cord injury keeps the ANS from working like it should.
- Medications such as vasodilators, antidepressants and diuretics.
- Alcohol use.
- Less fluid than normal in the body due to bleeding, diarrhea or vomiting.
This type of syncope usually causes changes in your blood pressure that cause it to drop by at least 20 mmHg (systolic/top number) and at least 10 mmHg (diastolic/bottom number) when you stand.
Autonomic Nervous System (ANS)
Postural Orthostatic Tachycardia Syndrome
Postural-Orthostatic Tachycardia Syndrome (POTS) is caused by a very fast heart rate (tachycardia) that happens when you stand after sitting or lying down. The condition is most common in women, but it can also affect men.
Cardiac syncope
Cardiac syncope is caused by a heart or blood vessel condition that affects blood flow to the brain. If you have cardiac syncope, it is important to see a cardiologist for treatment.
Cardiac syncope can be related to an abnormal heart beat (too fast or too slow) or another cardiovascular problem, such as hypertrophic cardiomyopathy (HCM), blocked blood vessels, valve
disease, heart failure, aortic dissection, pulmonary embolism or pulmonary hypertension.
How is syncope diagnosed?
If you have syncope, see your healthcare provider, who can refer you to a syncope specialist. The specialist will talk to you about your symptoms, review your medical history and do a physical exam.
You may have tests to help find out what is causing your syncope. These tests may include:
- Blood tests to check for anemia and metabolic changes.
- Electrocardiogram (EKG or ECG): A test that records the electrical activity of your heart to check for problems with your heart rate or rhythm.
- Exercise stress test: A test that uses an ECG to record your heart’s electrical activity while you exercise on a treadmill or stationary bike.
- Ambulatory monitor: A portable device that you wear for a period of time to collect information about your heart’s rate and rhythm.
- Echocardiogram: An ultrasound of your heart.
- Tilt table test: A test that records your blood pressure and heart rate as you lie on a table that is moved to different angles.
- Blood volume test: Measures how much blood you have in your body.
- Hemodynamic testing: A test to check the blood flow and pressure inside your blood vessels when your heart muscle contracts and pumps blood throughout the body.
- Autonomic reflex testing: A series of tests are done to check your blood pressure, blood flow, heart rate, skin temperature and sweating as you are exposed to different sensations. These measurements help identify nerve damage.
You may need other tests. If so, your doctor will explain what they are for and what to expect.
Getting your test results
Your referring physician will talk to you about your test results and treatment recommendations.
What treatments are available for patients with syncope?
Your treatment options depend on the cause of your syncope and the results of your evaluation and testing. The goal of treatment is to prevent episodes of syncope. Your healthcare team will work with you to create the best treatment plan possible.
Lifestyle and education
- Avoid or change the situations/“triggers” that cause a syncope episode, including alcohol and certain types of medicine.
- Teach your family and those close to you about symptoms that lead to syncope. Let them know to have you lie down and put your legs up if you start to feel symptoms.
- You may need to wear support garments or compression stockings to improve blood circulation.
- Make changes to your diet. You may need to eat small, frequent meals; increase your fluids and the amount of sodium and potassium in your diet; and avoid caffeine and alcohol.
- Be extra careful when you stand up if you tend to have symptoms when you get up after lying down.
- It may be helpful to sleep with extra pillows under your head of raise the head of the bed with risers.
- Biofeedback to help you control a fast heart rate.
Medications and procedures
- You may need to take medication, especially if you have orthostatic hypotension or an arrhythmia.
- If your syncope is caused by a problem with your heart’s structure, you may need to have surgery to correct it.
- If you have bradycardia (slow heart rate), you may need a pacemaker to keep your heart rate steady and regular. If you have a device and it is not working properly, you will need to be evaluated and have the device reprogrammed.
- If you have a fast ventricular arrhythmias or a history of sudden cardiac death (SCD), you may need an implantable cardiac defibrillator (ICD). This device constantly monitors your heart rate and rhythm and corrects it if needed.
How will syncope affect my life?
With the proper diagnosis and treatment, syncope can be managed and controlled. Once you have had an episode of syncope, there is about a 30% chance you will have another episode.
Your risk of another episode and how the condition affects you depends on several factors, including the cause of the problem, your age, gender and other medical problems you have. Talk to your doctor about any concerns or questions you have.
Check with your local drivers’ license bureau to see if you need to report that you have syncope.