What is a subcutaneous ICD?
A subcutaneous implantable cardioverter defibrillator (S-ICD) is an electronic device that constantly monitors your heart rhythm. When it detects a very fast, abnormal heart rhythm, it delivers energy to the heart muscle. This causes the heart to beat in a normal rhythm again.
An S-ICD is different from a traditional ICD because the wires (leads) that run from the device to your heart are implanted under your skin instead of through your veins. This allows the leads to be more easily removed and replaced.
Why do I need an S-ICD?
You may need an S-ICD if you have had, or are at high-risk of having, ventricular tachycardia or ventricular fibrillation. These are two life-threatening heart rhythms that cause the heart to beat very fast. These conditions can be fatal if you do not get immediate treatment.
You may need an S-ICD if you:
- Have had an episode of sudden cardiac arrest.
- Have had an episode of ventricular fibrillation.
- Have had at least one episode of ventricular tachycardia.
- Have had a heart attack and you are at high risk of having sudden cardiac arrest or sudden cardiac death.
- Have hypertrophic cardiomyopathy.
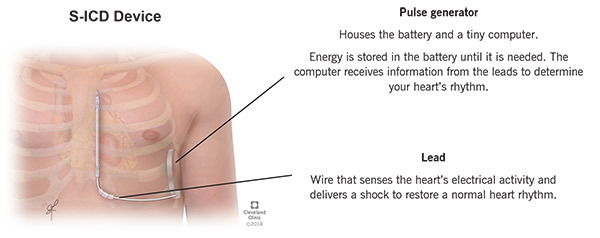
How does an S-ICD work?
The ICD monitors your heart rhythm, identifies abnormal, fast heart rhythms and sends a high-energy shock to the heart to restore a normal rhythm.
Is the ICD implant procedure safe?
A device implant is generally a very safe procedure. However, as with any invasive procedure, there are risks. Special precautions are taken to decrease your risks. Please discuss your specific concerns about the risks and benefits of the procedure with your doctor.
Where is the implant procedure performed?
In most cases, the implant procedure takes place in a special room in the Electrophysiology Lab.
Before the Procedure
What time should I report for my procedure?
The day before your scheduled procedure, please call 800.223.2273 and ask for Pager Number 21215, the EP scheduling nurse. Please call between 3 p.m. and 5 p.m. to find out what time you should arrive.
If your procedure is scheduled for a Monday, please call the Friday before. If your procedure is scheduled after a holiday, please call the last business day before the holiday.
Please do not call the Cleveland Clinic Operator or the Admitting Office for information about your procedure. We will notify you if there are any changes to your schedule.
Should I take my medications?
If you take Coumadin, the results of your INR test (a blood test to evaluate the blood clotting) must be within a suitable range before you can have the implant procedure. Your doctor may tell you to stop taking blood-thinning medications for a few days before the procedure.
Your doctor may also ask you to stop taking other medications, such as those that control your heart rate.
Do not stop taking any of your medications without first consulting with your healthcare provider. Ask your doctor which medications you should stop taking and when to stop taking them.
If you have diabetes, ask the nurse how to adjust your diabetes medications or insulin.
Can I eat before the procedure?
Eat a normal meal the evening before your procedure. However, DO NOT eat, drink or chew anything after midnight the night before your procedure. This includes gum, mints, water, etc.
Take medications with small sips of water. Do not swallow any water when you brush your teeth.
What should I wear?
Do not wear makeup or nail polish.
Wear comfortable clothes when you come to the hospital. You will change into a hospital gown for the procedure. We will give your clothes to the person who comes to the hospital with you.
Do not wear any jewelry (including wedding rings). Do not bring valuables to the hospital.
What should I bring?
You will not need a robe or toiletries when you first arrive. You may pack these items and have a family member keep your bag until after the procedure.
Bring a one-day supply of your prescription medications. Do not take these medications without first asking your doctor or nurse.
You may bring guided imagery or music and the appropriate player.
What happens before the procedure?
A nurse will help you get ready for the procedure.
You will lie on a bed and the nurse will start an intravenous (IV) line in a vein in your arm or hand. The IV is used to deliver medications and fluids during the procedure.
To prevent infection and to keep the device insertion site sterile:
- You will receive an antibiotic through the IV at the beginning of the procedure.
- We will shave one side of your chest (men).
- We will cleanse the area.
- We will cover you with sterile sheets (drapes) from your neck to your feet.
- You may have a soft strap across your waist and arms to keep your hands from touching the sterile area.
During the Procedure
Will I be awake?
You may get general anesthesia, which will cause you to "sleep" during the procedure, and you won’t feel anything.
Otherwise, you will get medication through your IV to help you relax and make you feel drowsy, but you will not be asleep during the procedure.
However, you will be "put to sleep" before the device is tested and a shock is delivered to your heart.
Will I be monitored?
Several monitors are used during the procedure to constantly check things like your heart rhythm and blood pressure.
How is the device implanted?
You will have 2 or 3 incisions that are closed with stitches that will dissolve. The S-ICD is implanted under the skin and fat in the side of your chest wall under your arm. A lead is tunneled under the skin to the middle of the chest near your breastbone, and then up towards your neck. The system is tested to make sure it is working as it should.
What will I feel?
If you do not get general anesthesia for the procedure, you will feel a burning or pinching sensation when the doctor injects the local numbing medication. Then, the area will become numb. You may feel a pulling sensation as the doctor makes a pocket in the tissue under your skin for the device. Please tell your doctor anything you feel. You should not feel pain. If you do, tell your nurse right away.
How long does the procedure last?
The device implant procedure may last 2 to 4 hours.
Monitors during the procedure
Defibrillator/pacemaker/cardioverter: Attached to one sticky patch placed on the center of your back and one on your chest. This allows the doctor and nurse to pace your heart rate if it is too slow, or deliver energy to your heart if the rate is too fast.
Electrocardiogram (EKG): Attached to several sticky electrode patches placed on your chest. Provides a picture of the electrical impulses traveling through your heart.
Blood pressure monitor: Connected to a blood pressure cuff on your arm. Checks your blood pressure throughout the procedure.
Oximeter monitor: Attached to a small clip placed on your finger. Checks the oxygen level of your blood.
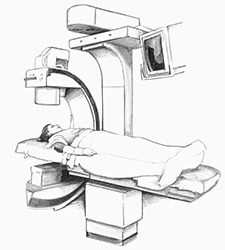
Fluoroscopy: A large X-ray machine will be positioned above you to help the doctors see the leads on an X-ray screen during the procedure.
After the Procedure
Will I have to stay in the hospital?
You may need to spend the night in the hospital, but many patients can go home a few hours after the procedure.
What should I expect during my recovery?
A special monitor, called a telemetry monitor, will continually monitor your heart rhythm. The telemetry monitor is a small box connected by wires to electrodes on your chest. Information about your heart rate and rhythm is displayed on screens at the nursing station.
What tests will be done after the procedure?
You will have a chest X-ray to check your lungs and the position of the device and lead. Afterward, you will go to the Device Clinic.
What happens at the Device Clinic?
You will sit in a reclining chair. Electrodes will be placed on your chest and connected to a computer. A nurse will place a small device (programmer) directly over the device to adjust the settings to meet your individual needs. Please tell your nurse if you have any symptoms.
Your doctor will get the results of the device check and make sure everything is working as it should.
How will I feel?
You may have discomfort at the device implant site during the first 48 hours after the procedure. Your doctor will tell you which medications you can take for pain relief. Please tell your doctor or nurse if your symptoms last a long time or are severe.
What information will I get before I leave the hospital?
Your doctor will talk to you about the results of the procedure and answer any questions you have. Please ask your doctor if you should keep taking the medications you took before your procedure.
You will get information about how to care for yourself after the procedure, including medication guidelines, wound care, activity guidelines, device care and maintenance, and a follow-up schedule. Also refer to the handout, "ICD Discharge Instructions".
ID card
You will get a temporary ID card that lists the type of device and leads you have, the device manufacturer, the date of the device implant and the doctor’s name who implanted the device. The device company will send you a permanent ID card within 3 months of the procedure. It is important to carry this card at all times in case you need medical attention.
Will I be able to drive myself home after the procedure?
No. For your safety, a responsible adult must drive you home. Please have your driver at the hospital by 10 a.m. on the day you go home.
Ask your doctor when you can start driving again.
When should I follow-up?
A follow-up appointment to check your ICD will be scheduled within 6 weeks after the device implant procedure. The appointment will be scheduled automatically and you will receive an appointment notice in the mail.
The ICD check is performed at the Device Clinic and takes about 15 to 30 minutes. The programmer will be placed over the device to check device settings, measure battery voltage and get information about any fast heart rhythms and/or therapies you received.
How long does the ICD last?
Your ICD can last 5 to 6 years. By keeping your follow-up appointments in the Device Clinic, your healthcare team can monitor the function of your device and anticipate when it needs to be changed.
Managing your condition
ICD therapy is only one part of a comprehensive treatment program. It is also important for you to take your medications, make changes to your diet, live a healthy lifestyle, keep your follow-up appointments and be an active member of your treatment team.
Action checklist
Before your procedure
- Call the scheduling nurse between 3 p.m. and 5 p.m. the day before the procedure to get your procedure time. Call 800.223.2273 and ask for Pager 21215.
- Do not eat or drink anything after midnight the night before the procedure.
- Talk to your doctor about the medications you should take before the procedure.
- Do not bring valuables.
After your procedure
- You may spend the night in the hospital.
- Your doctor will talk to you about your medications, homegoing instructions and follow-up schedule.
- Ask your doctor which daily medications you should take after your procedure. You may not need to take the same medications you did before the implant.
- Be sure to keep your follow-up appointments and make lifestyle changes as needed.
If you have questions
Please call the nursing staff in the Device Clinic at 216.444.6483 or 800.223.2273 ext. 46483 from 6:30 a.m. to 6:30 p.m., Monday through Friday. We prefer that you call between these hours if at all possible. You may also contact us via e-mail at devclin@ccf.org.
At other times, please call 800.223.2273 and ask for Pager 21215 to talk to the EP fellow on call.
If you have a change of address or phone number, please call us at 800.603.7169.