What is septal myectomy?
Septal myectomy is a surgical procedure that reduces the muscle thickening caused by hypertrophic cardiomyopathy (HCM).
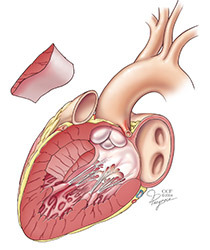
During the septal myectomy procedure, the surgeon removes a small amount of the thickened septal wall. This widens the area that the blood flows through as it goes from the left ventricle (bottom chamber of the heart) to the aorta. The procedure removes the obstruction and stops the mitral valve regurgitation caused by it. Many patients who have a septal myectomy no longer have symptoms after the procedure.
Cleveland Clinic has one of the largest surgical practices for treating patients with HCM. Our surgeons have been performing the septal myectomy procedure since 1967 and perform more than 150 myectomy procedures each year.
Hypertrophic cardiomyopathy (HCM) is a complex type of heart disease that causes the heart muscle to get thick, most often at the septum (the muscular wall between the left and right side of the heart), just below the aortic valve. If the septum becomes too thick, the passageway to the aorta becomes very narrow, which limits or blocks blood flow from the left ventricle to the aorta. This is called "outflow tract obstruction." The septal thickening ranges from a few millimeters to centimeters. The condition often causes mitral valve problems and affects repair techniques.
Is a septal myectomy right for me?
It is likely that more than 70% of patients with HCM have problems with blocked blood flow. The obstruction can range from mild to severe. If the obstruction is mild, treatment with medication may work well.
Your doctor may suggest a septal myectomy if you have symptoms of HCM after trying treatment with medications, or if you have a severe obstruction.
Septal myectomy is the safest, most successful and most durable procedure for patients with severe symptoms or severe obstruction. If you are elderly or have advanced medical problems, you may need a different procedure, called a percutaneous alcohol septal reduction.
To determine if septal myectomy is the right treatment option for you, you’ll need to see a Cleveland Clinic cardiologist. If you currently see a doctor outside of Cleveland Clinic, please call the Heart Center Resource and Information Nurse toll-free at 866.289.6911 or 216.445.9288 for more information about getting an evaluation at Cleveland Clinic.
If you are already being treated for a heart condition at Cleveland Clinic, ask your cardiologist if a septal myectomy is a treatment option for you.
If you are a good candidate for this surgery, Cleveland Clinic will review your medical information, including your medical records and various tests. A cardiologist will review your echocardiogram and cardiac catheterization results, and this review will be billed to your insurance. There is no charge for a review of your medical records.
What tests do I need before my surgery?
- An echocardiogram (echo) is needed to get information about how well your heart is working and the thickness of your septal wall. You may need to exercise or get medication during the test to help your doctor learn more about your obstruction and the health of your mitral valve.
- If you do not have an implantable defibrillator or pacemaker, you may need an MRI to check your mitral valve.
- A diagnostic cardiac catheterization within the past year.
- Routine blood tests, chest X-ray and an electrocardiogram (EKG).
Your Cleveland Clinic cardiologist will talk to you about these and other tests you need.
What are the possible risks of the surgery?
A septal myectomy is generally a very safe procedure. However, there are risks with all surgical procedures based on your age, other medical conditions you have and whether or not you are having another procedure along with a septal myectomy.
Some risks may include infection; irregular heart rhythm, such as ventricular arrhythmia; chest pain (angina); heart attack; stroke or death. We take every precaution to avoid these problems.
Your doctor will talk to you about the benefits and risks of the procedure as they relate to you, personally. Please ask your doctor any questions you have.
Also, please let your doctor know if you have concerns about lying flat on your back for 3 to 6 hours during the procedure.
What can I expect before the surgery?
You will have a presurgery appointment to meet your surgeon, anesthesiologist and ask any questions you have about the procedure. You will also get information about any tests you need (on the same or different day) and how to prepare for surgery.
If you are already in the hospital and your doctor recommends surgery, your healthcare team will give you information about the tests you need and how to prepare for surgery.
What happens during surgery?
Anesthesia: You will have general anesthesia for the surgery. The anesthesia team is led by a cardiothoracic anesthesiologist, and we use state-of-the-art equipment and monitors for your safety.
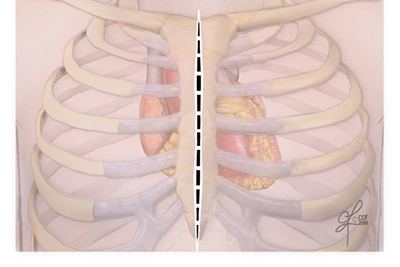
Incision: You will have a 6- to 8-inch incision down the center of your chest. This divides the sternum (breastbone) so your surgeon has direct access to your heart.
The surgeon does not make direct cuts in the heart muscle. Instead, he or she goes through the aortic valve to remove the thickened muscle. The area where the thickened muscle is removed heals on its own without stitches.
Heart-lung machine: The heart-lung (cardiopulmonary bypass) machine is used during surgery. It takes over the work of the heart so your surgeon can perform the procedure on a "still" heart.
Your blood goes through the heart-lung machine, which takes out carbon dioxide and adds oxygen before the blood is pumped back into your body. The heart-lung machine is turned off when the procedure is complete, and your heart will start working normally again.
Pacing wires: You will have temporary pacing wires and a chest tube to drain fluid. These are put in place before the sternum is closed with special wires. Internal, absorbable stitches are used to close the incision. You may need a temporary pacemaker to keep your heart rhythm steady. The pacemaker is attached to the wires.
How long does the procedure last?
The surgery lasts 3 to 6 hours.
What should I expect after surgery?
You can expect to stay in the hospital for about 5-7 days after surgery. This includes about 1-2 days in the intensive care unit (ICU) and 3 to 5 days in a step-down unit. Every patient has different needs, and your recovery time may be different.
While in the ICU, your healthcare team will closely monitor your heart, blood pressure, oxygen level and other vital signs.
Once you move to the nursing unit, you will work with a cardiac rehabilitation specialist to slowly become more active.
You may need an implantable cardioverter-defibrillator (ICD) if you have a serious abnormal heart rhythm. Your cardiologist will talk to you about the device and procedure if it is needed.
Your doctor may want you to have an electrophysiology (EP) study before you go home to check your heart rhythm.
You will get information (discharge instructions) about incision care, medications, activity and diet guidelines, signs of a problem and who to call after you go home. Please make sure you understand this information before you go home.
Medications after surgery: Keep taking the same medications you took before surgery until you see your cardiologist for a follow-up appointment. You may need to make changes to medications after the appointment. Do not stop or start taking any medication without asking your doctor.
Will My Symptoms Improve After Surgery?
Most patients have a significant improvement in symptoms and a better quality of life after surgery.
Recovery
A full recovery after septal myectomy surgery takes about 6 to 8 weeks. Most patients can drive 3 to 8 weeks after surgery. Your doctor will let you know when you can return to work and give you other information about your recovery.
Follow-up care
Your first follow-up appointment will be 5 to 7 days after you leave the hospital. You will see a surgical nurse clinician who will make sure there are no problems with your recovery. We will also call you to see how you’re doing.
Keep your regular follow-up appointments with your cardiologist. These are important to make sure your heart is working well and make sure you are taking the right types and amounts of medications. You may also need to have tests, like an echocardiogram, from time to time, in addition to exams.
During the first few months after surgery, you will also probably need a few visits with the doctor who referred you for surgery.
Even if you feel fine and are symptom-free, it is still very important to see your doctor as scheduled. Your doctor will let you know how often you need to be seen long-term, but in general, you will have at least 2 visits per year with your cardiologist.
Importance of making lifestyle changes
It is important to take all of your medications as prescribed and make healthy lifestyle changes to help prevent future health problems. Talk to your doctor about changes you need to make, such as:
- Eating a heart-healthy diet.
- Eating a low-sodium diet (ask your doctor what your daily sodium limit should be).
- Limiting the amount of fluids you have each day (ask your doctor what your limit should be).
- Not smoking or using tobacco/nicotine.
- Getting treatment for high cholesterol levels.
- Controlling high blood pressure and diabetes.
- Getting regular exercise.
- Reaching and staying at a healthy weight.
- Weighing yourself every day. Call your doctor if you gain more than 2 pounds in a day or 5 pounds in a week.
- Managing stress and anger.
- Joining a cardiac rehabilitation program.
- Seeing your doctor for all follow-up visits.
For More Information
- For information about hypertrophic cardiomyopathy or treatments, please contact the Miller Family Heart & Vascular Institute Information and Resource Center Nurse toll-free at 866.289.6911 or email us using the Contact Us form at: clevelandclinic.org/heart. We are happy to answer your questions.
- The Hypertrophic Cardiomyopathy Association (HCMA) is dedicated to providing support and education to those with HCM, their families and other healthcare professionals.
Contact: P.O. Box 306, Hibernia, NJ 07842
973.983.7429
E-mail: support@hcma-heart.com
Website: 4hcm.org