What is renal vein thrombosis?
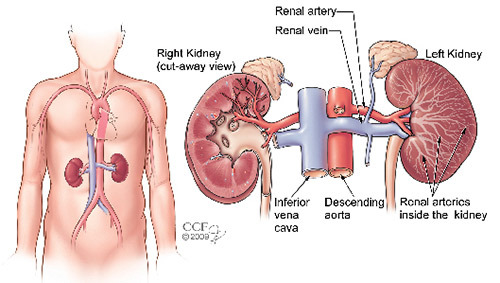
Renal vein thrombosis develops when a blood clot forms in the renal vein, which carries blood from the kidneys into the inferior vena cava and back to the heart. When the filtered blood leaving the kidney becomes blocked by renal vein thrombosis, the kidneys are unable to function properly. Kidney failure can occur without prompt treatment. The onset of renal vein thrombosis can be rapid (acute) or gradual.
Normally, kidneys rid the body of wastes by filtering the blood and eliminating the wastes into the bladder where they exit the body through the urine. During this filtration process, the kidneys also work to prevent excessive protein "leakage" into the urine, retaining the protein in the blood.
Blood clots in the renal veins are uncommon but when they do occur, there is a risk of pulmonary embolism. Pulmonary embolism is a dangerous condition resulting when the clot, or a portion of the clot, dislodges and follows the blood flow, traveling through the inferior vena cava all the way up to the lungs.
What are the symptoms of renal vein thrombosis?
Acute onset of renal vein thrombosis may cause pain in the lower back and side, fever, bloody urine, decreased urine output and sometimes high blood pressure and kidney failure. Some patients have no symptoms.
What causes renal vein thrombosis?
Renal vein thrombosis can be caused by injury to the abdomen or back, as a result of malignant kidney tumors growing into the renal vein. Renal vein thrombosis can also be caused by hypercoagulable states, or as a result of kidney diseases causing degenerative changes in the cells of the renal tubules (nephrotic syndrome).
Hypercoagulable states and thrombophilia include inherited, or acquired, abnormalities in the blood clotting system and/or bone marrow. These abnormalities can increase a person’s risk for developing excessive or abnormal blood clots in unusual locations, including the renal veins.
Nephrotic syndrome occurs when the kidneys allow excessive "leakage" of protein into the urine. Nephrotic syndrome is marked by abnormally low levels of a blood protein called albumin (hypoalbuminemia), high cholesterol levels in the blood (hypercholesterolemia), fluid retention, high blood pressure and swelling (edema).
Nephrotic syndrome is not a disease itself but usually occurs as a complication of other medical conditions, such as diabetes and diseases which lead to kidney inflammation (glomerulonephritis).
When the onset of the disorder is gradual, there is a slow decrease in kidney function and protein appears in the urine. These patients may not have any symptoms, unless they develop kidney failure.
How is renal vein thrombosis diagnosed?
A physician makes the diagnosis of renal vein thrombosis based on the presence of symptoms and the results of a medical examination and diagnostic tests.
Urine tests and blood tests
Urine tests and blood tests are usually performed, but they are not specific for the diagnosis. The urine test may detect abnormally large levels of protein, and blood tests may indicate abnormally high levels of cholesterol. Specific blood tests for hypercoagulable states and thrombophilia are also non-diagnostic, but may be performed once the diagnosis has been confirmed.
Vascular ultrasound
Vascular ultrasound is a non-invasive ultrasound method used to examine blood circulation and detect blood flow within the veins, as well as blood clots. During a vascular ultrasound, an ultrasound transducer (small hand-held device) is placed over the area being examined.
The transducer generates high-frequency sound waves through the tissues. The sound waves are reflected back from moving blood cells within the blood vessels, allowing the examiner to determine whether blood flow is present or not. Because the renal veins are located deep within the abdomen, vascular ultrasound often can not be used to detect a blood clot in the renal veins, but it may be very helpful in determining whether the renal veins are patent (open) or not.
CT Scans, MRI and Venography
The most accurate tests for the diagnosis of renal vein thrombosis are:
- Computed tomography scans (CT scans).
- Magnetic resonance imaging (MRI).
- Venography (catheterization of the renal veins).
These tests can be used to identify narrowing or blockage in the renal veins, and are also helpful to determine whether such blockages are caused by conditions within the veins (blood clots) or by surrounding tumors which may be invading the renal veins or squeezing them shut. Renal venography (also called renal angiography) may need to be performed when other less invasive tests do not provide enough information to make a proper diagnosis.
During renal venography, a catheter (long, thin tube) is inserted into the femoral vein in the groin area, and threaded up into the inferior vena cava to reach the veins of each kidney. Contrast material (dye) is then injected through the catheter into each vein while X-rays are taken.
Kidney Biopsy
If the renal vein thrombosis is caused by nephrotic syndrome, a biopsy (sample of kidney tissue) may need to be obtained to better evaluate the underlying kidney disease that is causing the excessive "leakage" of protein into the urine.
A kidney biopsy usually can be performed percutaneously (through the skin, no open procedure) with a special needle under local anesthetic. During the biopsy procedure, you will lie on your stomach.
The doctor will mark the entry site, clean the area, and inject a local painkiller. The doctor will use a locating needle and x-ray or ultrasound equipment to guide the biopsy needle to the right location to collect the tissue sample.
The doctor may ask you to hold your breath while the tissue samples are being collected. The doctor may need three or four passes to collect the needed samples. The entire procedure usually takes about an hour.
What treatments are available for patients with renal vein thrombosis?
One of the major goals of treatment is to prevent the blood clots from detaching and moving into the lungs, causing a potentially very serious complication called pulmonary embolism.
Hospital admission and intravenous delivery of anticoagulant medications (also referred to as "blood thinners"), such as various types of heparins, are necessary to prevent pulmonary embolism, to prevent existing blood clots from enlarging and extending into the inferior vena cava, as well as to prevent the formation of new blood clots.
In some specific cases, clot-busting medications (thrombolytic drugs) such as tissue plasminogen activator (t-PA) may be given to help dissolve the renal vein clots. Clot-buster medications must be administered properly through several specifically timed intravenous infusions, according to a rigid protocol established for each individual drug and based on the body weight of each patient. In patients with renal vein thrombosis, these medications appear to be most effective when given through a catheter placed within the inferior vena cava or renal vein. Bedrest or limited activity may be recommended for a brief period.
If there is a tumor causing the blockage of the renal vein, blood flow can often be restored by removing the tumor. This is done through an incision in the renal vein, or an incision in the vena cava, the main vein in the body that the renal veins drain into. In rare situations, the renal vein will need to be removed along with the tumor. In some cases, the resected portion of renal vein can be bypassed or reconstructed with part of a vein from another site in the body.
After hospital discharge, patients with renal vein thrombosis usually take an oral anticoagulant ("blood thinner") medication called warfarin for a period that varies from a few months to many years. The total duration of therapy is dependent upon the underlying disease or condition that caused the abnormal blood clot formation in the renal veins.
What type of follow-up do I need?
Most cases of renal vein thrombosis resolve without any permanent damage. Death from renal vein thrombosis is rare, and is often caused by the blood clot detaching and lodging in the lungs or heart.
Patients should follow-up closely with their physicians to monitor their condition, as well as keep all laboratory test appointments to monitor the effectiveness of prescribed medications.