Disease of the arteries that supply blood to the kidneys – a condition known as renal artery stenosis – is less common than the more familiar form of atherosclerosis, peripheral arterial disease, but is equally serious.
What is renal artery disease?
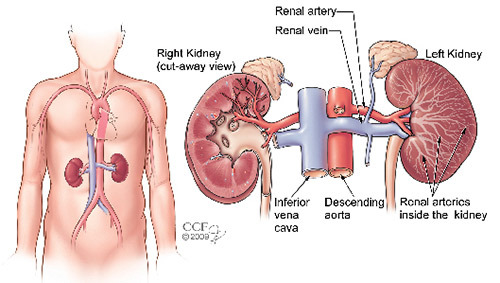
Like the atherosclerosis that affects the arteries of the legs (peripheral artery disease), renal artery disease is caused by the buildup of plaque in the arteries that lead to the kidneys. Plaque is made up of fats and cholesterol, and as it accumulates in the renal arteries, it causes the arteries to stiffen and narrow, which blocks the flow of blood to the kidneys. Obstructions (blockages) in the renal arteries, known as renal artery stenoses, can cause poorly controlled high blood pressure, congestive heart failure, and kidney failure.
What causes renal artery disease?
Renal artery disease is often related to peripheral artery disease (atherosclerosis in arteries outside the heart) or coronary artery disease. Atherosclerotic renal artery disease is the most common form of this condition, accounting for more than 80 percent of all renal artery diseases. The balance is generally caused by fibromuscular dysplasia, a congenital disorder that causes thickening of the artery walls without plaque build-up.
The kidneys play an important role in regulating blood pressure by secreting a hormone called renin. If the renal arteries are narrowed or blocked, the kidneys cannot work effectively to control blood pressure. Persistent or severe high blood pressure is a common symptom of renal artery stenosis.
What are the symptoms?
High blood pressure that is not controlled by medications and lifestyle changes, including diet and exercise, may be a symptom of renal artery disease. Symptoms of renal artery disease may also include episodes of fluid retention or congestive heart failure. In some cases, renal artery disease may be entirely asymptomatic (not associated with any symptoms).
In severe cases, renal artery disease may lead to kidney failure. Symptoms of kidney failure include weakness, shortness of breath and fatigue.
What are the risk factors?
Many of the risk factors for renal artery disease are the same as those for atherosclerosis in other parts of the body, such as coronary artery disease and peripheral arterial disease. Risk factors for renal artery disease include: age over 50, diabetes, high cholesterol, smoking, high blood pressure, a history of coronary artery disease or peripheral arterial disease, a family history of renal artery disease and neurofibromatosis.
Diagnosis
Once a diagnosis of renal artery disease is suspected, a diagnostic test is generally ordered to evaluate the renal arteries for the presence of significantly narrowed areas. Tests that can be used to diagnose renal artery stenosis include abdominal duplex ultrasound, magnetic resonance angiography (MRA), computed tomography (CTA), or nuclear medicine testing (captopril renal scanning). In some cases, an invasive angiogram may be recommended to evaluate the renal arteries.
Treatment choices
In nearly half of patients, untreated renal artery disease gets progressively worse and can lead to kidney failure. In one large study at Cleveland Clinic, obstruction of the arteries progressed in 44 percent of untreated patients; in 16 percent of those, total occlusion occurred. For unknown reasons, women are at higher risk for disease progression than men.
Like treatment for heart disease, there are many treatments available for renal artery disease. The right treatment for an individual depends on the severity of the disease and the person’s medical history.
Medical therapy
All patients with renal artery disease require treatment for cardiovascular risk factors (such as high blood pressure, high cholesterol, diabetes) and lifestyle changes such as weight reduction, smoking cessation, exercise and a low-salt and low-fat diet. Medication to lower blood pressure is an important part of treatment, along with careful monitoring of the response to the blood pressure medications to be sure the blood pressure is lowered to the treatment goal. Regular follow-up every 4 to 6 months will be part of the treatment plan so your physician can monitor your condition.
For some patients with significant narrowing of the renal arteries, particularly patients with narrowed areas in the renal arteries on both sides of the body, or those with severe symptoms, a procedure may be recommended to open up the blocked arteries to restore circulation. In some cases, opening the blocked arteries may improve kidney function and may improve control of high blood pressure. Not surprisingly, the techniques used to open blocked renal arteries are very similar to those used to treat blocked coronary arteries.
Renal angioplasty
A small catheter – a long, thin tube – carrying a tiny balloon is inserted through a small puncture in the groin and guided by an X-ray to the kidney artery. When the catheter is guided to the narrowed part of the artery, the balloon is inflated. As it expands, it compresses the plaque against the artery walls, re-opening the vessel for blood to flow through. Once the artery is open, the physician may insert a stent at the site to keep the artery open and support the arterial wall.
In carefully selected patients, renal angioplasty improves blood pressure and kidney function with minimal risk. It can be done as an outpatient procedure or with only an overnight stay, does not require general anesthesia and has a short recovery time.
Surgical treatment
With the development of new and improved types of stents, angioplasty with stenting is the preferred treatment for renal artery disease. But, in certain cases, surgical treatment may be necessary to restore blood flow to the kidney and preserve kidney function. Surgical treatments for renal artery disease include:
Endarterectomy, during which a vascular surgeon removes the diseased inner lining of the artery and the plaque deposits.
Bypass procedure, which involves using a segment from another artery or vein to construct a detour around the blocked area of the renal artery. The most commonly used technique creates a bypass from the abdominal aorta (the large artery in the abdomen) to the kidney using a segment from the saphenous vein in the leg or the hypogastric artery from the abdomen.
Conclusion
There is no single best treatment for renal artery disease. The treatment that is best for you will depend on the severity of your disease, the location of the blockages in the arteries, your symptoms, and overall health, and many other factors. Because of the complex nature of renal artery disease, you should consult an experienced vascular specialist who works with a team of other specialists such as kidney doctors.