What is peripheral artery disease (PAD)?
Peripheral artery disease (PAD) affects the blood vessels (arteries) that carry oxygen and nutrient-rich blood to your arms and legs.
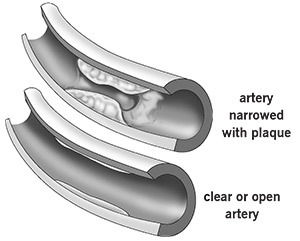
Healthy arteries have a smooth lining that prevents blood clots and promotes steady blood flow. But, plaque can gradually build up on the inside walls of the arteries. This condition is called atherosclerosis or "hardening of the arteries." Plaque is made of fat, cholesterol and other substances (inflammatory cells, proteins and calcium) that float through the bloodstream. The plaque build-up can cause your arteries to become narrowed or blocked, which blocks blood flow to your organs and other tissues. Without enough blood and nutrients, the organs and tissues become damaged, and the damage can lead to serious problems.
What are the symptoms of peripheral artery disease?
It can take many years for PAD to develop, and you may not have symptoms until later in life. Many people don’t notice symptoms until the artery is narrowed by 60% or more. Many people with PAD do not have any symptoms.
Intermittent claudication is the name for the leg discomfort, pain and cramping that is felt while active (when muscles need more blood) but that goes away when resting (when less blood flow is needed). For many people, it is one of the first symptoms of PAD. The pain often affects the calf, but it can also be felt in the buttocks and thighs. You may also feel numbness, weakness, heaviness or fatigue in your leg muscles when you walk, but not when resting. The pain can be bad enough to interfere with walking.
Other symptoms of advanced PAD may include:
- A burning or aching pain in the feet and toes while resting, especially at night while lying flat.
- Cool skin in the feet.
- Redness or other color skin color changes.
- More frequent infections.
- Toe and foot sores that do not heal.
What are the risk factors for PAD?

There are several factors that increase your risk of getting PAD:
- Smoking.
- Diabetes.
- Age: In the United States, people 50 and older have an increased risk for PAD.
- Race: African Americans are twice as likely to have PAD compared with other racial groups.
- A personal or family history of heart or blood vessel disease.
- High blood pressure (hypertension).
- High cholesterol (hyperlipidemia).
How do I know if I have PAD?
Talk to your doctor if you have symptoms of PAD so you know what the problem is and get treatment. Early detection and treatment help prevent complications like heart attack and stroke.
Your doctor will examine you and talk to you about your medical history and risk factors. You may need tests to see if you have PAD and how bad it is.
- The ankle/brachial index (ABI) compares the blood pressure in your lower legs to the blood pressure in your arms. During this test, blood pressure cuffs are placed on your arms and legs. The cuffs are inflated and a hand-held device (called a Doppler) is used to listen to the blood flow. The ABI screening checks to see how much blood is flowing to your legs and feet. If you have PAD, the pressure will be lower in those areas.
- A pulse volume recording (PVR) measures changes in the amount of blood in your legs and helps locate blockages. During this test, a blood pressure cuff is placed on your arm and multiple cuffs are placed on your legs. You will lie down and the cuffs will be slightly inflated. As blood pulses through your arteries, the blood vessels expand, causing an increase or decrease in the amount of air in the cuff. The changes are recorded. Your blood pressures are measured before and after you exercise on a treadmill. This helps determine if your pain is due to PAD.
- A vascular ultrasound checks your blood flow. A small hand-held device called a transducer is placed on the skin over the artery to be examined. The transducer sends out sound waves (you won’t hear them) that bounce off the artery. These sound waves are recorded, and an image of the vessel is created. This test can be used to find a blockage in an artery.
Other tests you may need are angiography, CT scan or MRI.
During angiography (also called arteriography), a special dye is injected into the blood vessels. X-ray pictures of the inside of the blood vessels are taken to check blood flow and look for blockages.
A CT scan uses X-rays taken from many angles in a very short period of time. The images are collected by a computer and cross-sectional "slices" of the blood vessel are shown on the monitor.
MRI uses powerful magnets to create images of your organs and blood vessels.
What treatments are available?
Treatment for patients with PAD include lifestyle changes, medications and interventional procedures. Your doctor will talk to you about the best treatments for you.
Lifestyle Changes. The first steps in treatment include making lifestyle changes to reduce your risk factors. Changes you can make to manage your condition include:
- Quit smoking. Ask your doctor about smoking cessation programs available in your community.
- Dietary changes. If you are overweight or obese, your doctor may recommend changes to your diet to help you lose weight, which takes pressure off your legs.
- Exercise. Begin a regular exercise program, such as walking. Regular walking, over time, will allow you to walk longer without feeling pain.
- Manage other health conditions, such as high blood pressure, diabetes or high cholesterol.
- Practice good foot and skin care to prevent infection and reduce the risk of complications.
Medications. You may need to take medications to control conditions like high blood pressure or high cholesterol.

You may need an antiplatelet medication to reduce your risk of heart attack and stroke.
Cilostazol (Pletal) can help improve walking distance. This medication can help people with intermittent claudication exercise longer before they have leg pain and to walk longer before they need to stop because of the pain. Your doctor will let you know if this medication is a treatment option.
Interventional procedures. If you have more advanced PAD, you may need an interventional procedure such as angioplasty to open the artery and have a stent (small, mesh tube) placed to keep the artery open.
Sometimes surgery, such as peripheral artery bypass surgery, is needed to reroute blood flow around the blockage in the blood vessel.
New therapies are being researched. Talk to your doctor about other possible treatment options.
Foot care guidelines

Every day, look at your legs, tops and bottoms of your feet, and the areas between your toes. Check for blisters, cuts, cracks, scratches and other sores. Also check for redness, increased warmth, ingrown toenails, corns and calluses. If you have trouble, use a mirror or have a family member look at the area for you.
Once or twice a day, use moisturizing cream or lotion on your legs and feet to prevent dry skin and cracking. Do not apply lotion between your toes or in areas where you have an open sore or cut. If your skin is extremely dry, use the moisturizing cream more often.
Care for your toenails regularly. Cut your toenails after bathing, when they are soft. Cut toenails straight across and smooth with a nail file.
If you have diabetes, it is important to see a podiatrist.
Do not self-treat corns, calluses or other foot problems. Go to a podiatrist for treatment.
Do not wait to get treatment for a minor foot or skin problem.
Ask your doctor if you have any questions about foot care.
Walking program
Vascular Medicine and Preventive Cardiology and Rehabilitation offer a structured supervised walking program to help you succeed and get the most out of your exercise efforts. Please call 216.444.4420 or 800.223.2273 ext. 4420 to make an appointment.
What are the conditions associated with PAD?
Without treatment, PAD can lead to serious health problems, including:
- Heart attack: Permanent damage to the heart muscle caused by a lack of blood supply to the heart for an extended time.
- Stroke: Interruption of the blood flow to the brain.
- Transient ischemic attack (TIA): A temporary interruption in the blood supply to the brain.
- Renal artery disease or stenosis: Narrowing or blockage of the artery that supplies blood to the kidney.
- Amputation: Removal of part or all of the foot or leg (rarely the arm), especially in people who also have diabetes.
Can PAD be cured?
There is no cure for PAD. Quitting smoking, exercising regularly and managing your risk factors — such as diabetes, high cholesterol and high blood pressure — can keep PAD from getting worse.