The pericardium
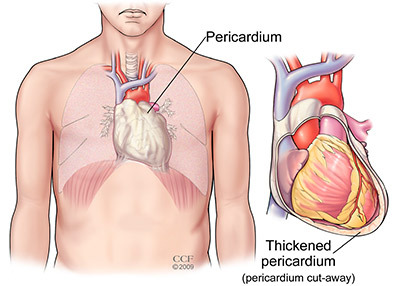
The pericardium is a thin, two-layered, fluid-filled sac that covers the outside of your heart. It keeps your heart lubricated, protects your heart from infection and disease, and holds your heart inside your chest. The pericardium also keeps your heart from getting too big when it gets more blood than usual. This helps your heart work the best it can.
What is pericarditis?
Pericarditis is an inflammation of the pericardium. Pericarditis is usually acute, which means it starts suddenly and may last up to several months. The condition usually clears up after 3 months, but sometimes attacks can come and go for years. When you have pericarditis, the membrane around your heart is red and swollen, like the skin around a cut that becomes inflamed. Sometimes there is extra fluid in the space between the pericardial layers, which is called pericardial effusion. Pericarditis can affect anyone, but it is most common in men aged 16 to 65. About 15% to 30% of patients with pericarditis have repeat episodes of pericarditis that come and go for many years.
If you have any symptoms of acute pericarditis, call your doctor right away. If you feel your symptoms are a medical emergency, call 911 right away.
What are the symptoms of pericarditis?
Pericarditis can cause chest pain that:
- Is sharp and stabbing (caused by your heart rubbing against the pericardium).
- May get worse when you cough, swallow, take deep breaths or lie flat.
- Feels better when you sit up and lean forward.
You also may feel the need to bend over or hold your chest to breathe more comfortably.
Other symptoms include:
- Pain in your back, neck or left shoulder.
- Swelling in your legs, feet, ankles or abdomen.
- Trouble breathing when you lie down.
- A dry cough.
- Anxiety.
- Feeling very tired/fatigue.
- Heart palpitations/abnormal heart beat that can feel like a racing/pounding heart beat or skipped beats/fluttering in your chest.
Constrictive pericarditis is a very serious type of pericarditis where the pericardium gets hard and/or thick over time. This keeps the heart muscle from expanding and keeps your heart from working like it should. Your heart can become compressed, which causes blood to back up into your lungs, abdomen and legs, and leads to swelling. Symptoms include swelling in your legs, feet or abdomen; shortness of breath; and heart palpitations. If you have these symptoms, schedule an evaluation with a cardiologist.
What are pericardial effusion and cardiac tamponade?
Pericardial effusion means there is too much fluid between your heart and pericardium. If the build-up causes pressure on your heart that keeps it from working like it should, it is called cardiac tamponade. Cardiac tamponade can also cause your blood pressure to drop. Cardiac tamponade is a life-threatening situation, and the fluid must be drained right away.
What causes pericarditis?
- Viral pericarditis is caused by a complication of a viral infection, most often a "stomach".
- Bacterial pericarditis is caused by a bacterial infection, including tuberculosis.
- Fungal pericarditis is caused by a fungal infection.
- Parasitic pericarditis is caused by an infection from a parasite.
- Some autoimmune diseases, such as lupus, rheumatoid arthritis and scleroderma can cause pericarditis. Other causes of pericarditis include a chest injury, such as after a car accident (traumatic pericarditis), other health problems such as kidney failure (uremic pericarditis), tumors, genetic diseases such as Familial Mediterranean Fever (FMF), and in rare cases, medications that suppress the immune system.
- The cause of pericarditis is often unknown. This is called idiopathic pericarditis.
Your risk of pericarditis is higher after a heart attack, heart surgery, radiation therapy or a percutaneous treatment, such as cardiac catheterization or radiofrequency ablation (RFA). This is because your body can make a mistake as it responds to the procedure and causes your pericardium to become inflamed. It can sometimes take several weeks for symptoms of pericarditis to develop after bypass surgery.
How is pericarditis diagnosed?
Sharp pain in your chest/back of your shoulders and trouble breathing are two major clues that you may have pericarditis rather than a heart attack. Your doctor will talk to you about your symptoms and medical history, including procedures and health problems that could increase your risk of pericarditis.
Your doctor will listen to your heart. Pericarditis can cause a rubbing or creaking sound, caused by the rubbing of the inflamed lining of the pericardium. This is called the "pericardial rub," and is best heard when you lean forward, hold your breath and breathe out. Depending on how bad the inflammation is, your doctor may also hear crackles in your lungs, which are signs of fluid in the space around your lungs or extra fluid in the pericardium.
Cleveland Clinic imaging specialists in the Center for the Diagnosis and Treatment of Pericardial Diseases often use a variety of ways to check for pericarditis and any complications. You may need one or more tests, such as:
- Chest X-ray to see the size of your heart and any fluid in your lungs.
- Electrocardiogram (ECG/EKG) to look for changes in your heart rhythm. About half of all patients with pericarditis have a distinct sequence of four patterns. Some changes are temporary, and some patients do not have any changes.
- Echocardiogram (echo) to see how well your heart is working and check for fluid or pericardial effusion around the heart. An echo will show the classic signs of constrictive pericarditis, including a stiff or thick pericardium that restricts the heart’s normal movement.
- Cardiac MRI to check for extra fluid in the pericardium, pericardial inflammation or thickening, or compression of the heart. A contrast agent is used during this highly specialized test.
- CT scan to look for calcium in the pericardium, fluid, inflammation, tumors and disease around the heart. Iodine dye is used during the test to get more information about the inflammation. This is an important test for patients who may need surgery for constrictive pericarditis.
- Cardiac catheterization to get information about the filling pressures in the heart. This is used to confirm a diagnosis of constrictive pericarditis.
- Blood tests can be used to make sure you are not having a heart attack, to see how well your heart is working, test the fluid in the pericardium and help find the cause of pericarditis. If you have pericarditis, it is common for your sedimentation rate (ESR) and ultra sensitive C reactive protein levels (markers of inflammation) to be higher than normal. You may need other tests to check for autoimmune diseases like lupus and rheumatoid arthritis.
What treatments are available for patients with pericarditis?
Medications
Treatment for acute pericarditis may include medication for pain and inflammation, such as ibuprofen and aspirin. Depending on the cause of your pericarditis, you may need an antibiotic or antifungal medication.
If your symptoms are severe, last longer than 2 weeks, or clear up and then return, your doctor may also prescribe an anti-inflammatory drug called colchicine. Colchicine can help control the inflammation and prevent pericarditis from returning weeks or even months later.
If you need to take large doses of ibuprofen, your doctor may prescribe medications to ease gastrointestinal symptoms. If you take large doses of nonsteroidal anti-inflammatory drugs (NSAIDs), you will need frequent follow-up appointments to check for changes in your kidney and liver function.
If you have chronic or recurrent pericarditis, you may need to take NSAIDs, colchicine or prednisone for several months or years. Your doctor will slowly taper your doses of the medications.
A diuretic (“water pill”) usually helps get rid of the extra fluid caused by constrictive pericarditis. If you develop a heart rhythm problem, your doctor will talk to you about treatment.
Your doctor may also talk to you about treatment with other medications, such as rilonacept, anakinra, azathioprine, methotrexate or IV human immunoglobulins.
Other treatments
Most times, medications are the only treatment needed for patients with pericarditis. But, if fluid builds up in the pericardium and compresses the heart, you may need a procedure called pericardiocentesis. A long, thin tube called a catheter is used to drain the extra fluid. The catheter and a needle are guided to the pericardium with the use of echocardiography. If the fluid cannot be drained with the needle, you will need a surgical procedure called a pericardial window.
If you have constrictive pericarditis, you may need to have some of your pericardium removed. The surgery is called a pericardiectomy.
Surgery is not usually used as treatment for patients with recurrent pericarditis, but your doctor may talk to you about it if other treatments aren’t successful.
Will pericarditis affect me in the long-term?
After you recover from pericarditis, you should be able to return to your normal activities without concern. Your doctor will talk to you about what to expect.
How do I find a doctor who can diagnose my condition and provide treatment?
The Center for the Diagnosis and Treatment of Pericardial Diseases in the Sydell and Arnold Miller Family Heart, Vascular and Thoracic Institute is a specialized center that includes a multidisciplinary group of specialists, including cardiologists, cardiac surgeons and nurses. These experts use a comprehensive approach to diagnosis and provide treatment for pericarditis. Depending on a patient’s medical background, other specialists, such as rheumatologists and infectious disease experts, may also be involved in the plan of care.
Call 800.659.7822 to schedule an appointment. Let the appointment office know you are having acute symptoms and ask for the name of the doctor you will be seeing.
Pericarditis terms
Acute pericarditis: Sudden inflammation of the pericardium. Symptoms also develop suddenly.
Cardiac tamponade: Severe compression of the heart that keeps it from working like it should. Cardiac tamponade is a medical emergency that requires prompt diagnosis and treatment.
Chronic pericarditis: Inflammation of the pericardium that lasts for three months or longer after the initial acute attack.
Constrictive pericarditis: A severe form of pericarditis in which the inflamed layers of the pericardium stiffen, develop scar tissue, thicken and stick together. Constrictive pericarditis interferes with the normal function of the heart.
Incessant pericarditis: Inflammation of the pericardium that lasts more than 4-6 weeks, but less than 3 months.
Infectious pericarditis: Pericarditis that develops as the result of a viral, bacterial, fungal or parasitic infection.
Idiopathic pericarditis: Pericarditis that does not have a known cause.
Pericardium: The thin, two-layered, fluid-filled sac that covers the outer surface of the heart.
Pericardial effusion: Excess fluid build-up in the pericardium.
Pericardial window: A minimally invasive surgical procedure performed to drain fluid that has accumulated in the pericardium. This surgical procedure involves a small chest incision through which an opening is made in the pericardium.
Pericardiectomy: Surgical treatment of pericarditis that involves the removal of a portion of the pericardium.
Pericardiocentesis: A procedure performed to drain excess fluid from the pericardium with a catheter.
Recurrent pericarditis: Repeat episodes of inflammation of the pericardium with improvement after the first episode and no symptoms for at least 4-6 weeks between episodes.
Traumatic pericarditis: Pericarditis that develops as the result of injury to the chest, such as after a car accident.
Uremic pericarditis: Pericarditis that develops as the result of kidney failure.