What is patent ductus arteriosus?
Patent ductus arteriosus (PDA) is a congenital heart defect – a heart problem that is present at birth.
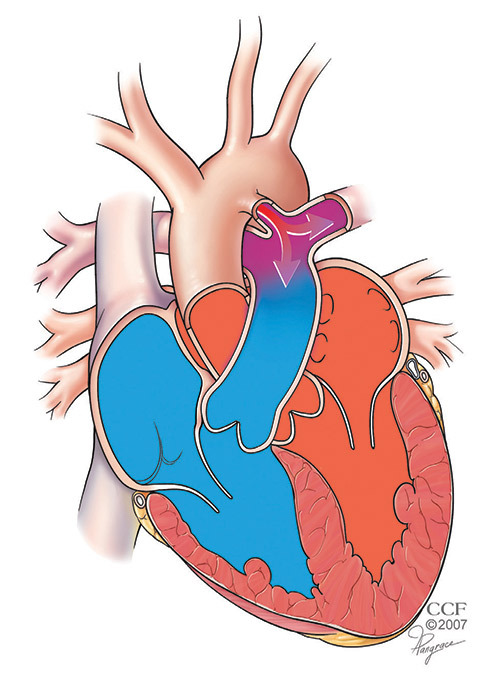
Patent ductus arteriosus is an abnormal connection between the aorta and the pulmonary artery in the heart. The pulmonary artery carries blood from the heart’s right lower chamber (ventricle) to the lungs, where it is loaded up with oxygen. From the lungs, the blood returns to the heart’s left ventricle and is pumped out through the aorta to the body.
While the baby is in the womb, the aorta and the pulmonary artery are connected by a temporary blood vessel, the ductus arteriosus. This vessel lets blood flow directly to the baby’s aorta, bypassing the lungs. Blood does not need to go through the baby’s lungs because he/she gets oxygen from the mother’s circulation.
After birth, the ductus arteriosus usually seals off so that blood from these two vessels does not mix. In patients with PDA, the ductus arteriosus stays open (patent), and blood can flow from the aorta into the pulmonary artery.
How common is PDA?
Patent ductus arteriosus is one of the most common congenital heart defects. About 3,000 newborns are diagnosed with PDA each year in the United States. Premature babies are more likely to have PDA, and the condition occurs twice as often in girls as in boys.
What problems does PDA cause in older children and adults?
Most patients with PDA are diagnosed and treated when they are infants, so this is a relatively rare congenital heart defect in older children and adults. When this is the case, the PDAs are usually small to moderate.
Symptoms of untreated PDA include shortness of breath and heart palpitations. Older children and adults with a PDA have a high risk of getting bacterial endocarditis (an infection of the lining of the heart, valves, or arteries), an enlarged heart (cardiomyopathy), pulmonary hypertension (high blood pressure in the lungs), congestive heart failure, and death.
How is PDA diagnosed in older children and adults?
A doctor may suspect a PDA if you have shortness of breath, heart palpitations and a heart murmur that is heard through the stethoscope. Testing is needed to confirm you have a PDA.
Testing may include:
- An echocardiogram: An ultrasound of the heart that clearly shows the heart’s structure and size. Doppler can also be used to check the direction and speed of bloodflow through the PDA.
- An electrocardiogram (ECG): A recording of the heart’s electrical activity that shows any problems with your heart rhythm.
- Oximetry: A simple test to measure the amount of oxygen in your blood. A clip is placed on your finger or toe to get the oxygen level reading. The test can help your doctor know if you have pulmonary hypertension that has caused blood to flow backwards through the PDA.
What treatments are available for older children and adults with a PDA?
Your doctor will likely recommend closing the PDA, unless you have advanced pulmonary hypertension. Closure can reduce complications from the PDA, restore normal blood circulation, eliminate symptoms and reduce your risk of dying.
More than 95 percent of patients with a PDA can have the defect closed using a catheter-based procedure. You may need to have surgery if you have a very large PDA.
Video-assisted thoracic surgical (VATS) repair is a minimally invasive surgery used to close PDAs. The surgery is done through a small incision in the chest, and a tiny camera helps guide the surgeon through the procedure.
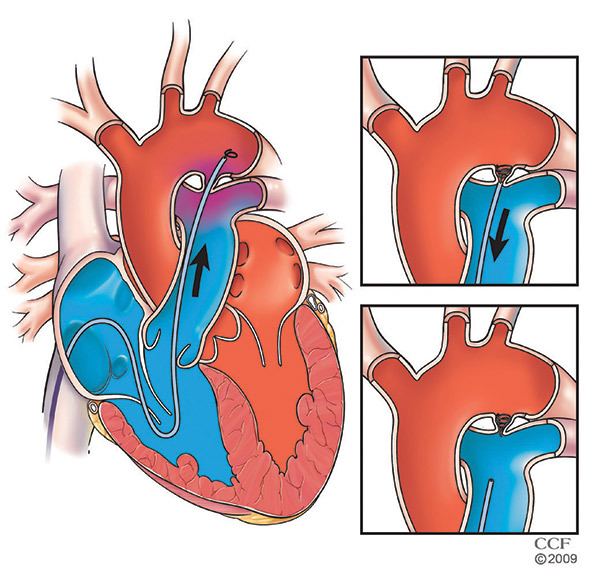
Transcatheter occlusion is the least invasive and preferred option to close a PDA. The procedure involves a catheter, which is used to place one or more coils or a fitted plug in the area of the PDA. The device opens up and blocks the opening. This technique results in a completely blocked defect within 1 year of the procedure for more than 85 percent of patients who have it done.
Repairing a PDA in an adult is a more complicated procedure than performing the procedure in children. Adults with a PDA should be under the care of an adult congenital heart disease specialist with experience in treating patients with PDAs. The specialist will recommend a plan of care after a complete evaluation that considers factors such as the size of the PDA, complications related to the PDA and your overall health.
You should continue to see your specialist for follow-up care after the closure procedure.
How will I feel after PDA repair?
Closure of a PDA restores normal circulation to the heart and reduces your risk of complications from the defect. But you may have permanent damage caused by the PDA, such as congestive heart failure, pulmonary vascular disease or calcium deposits where the PDA was.
You will likely need to take antibiotics for 6 months after a closure procedure to reduce your risk of getting endocarditis. Depending on the success of the closure procedure, you may need to continue taking antibiotics for the the rest of your life to prevent infection.
Where can I learn more or find a specialist?
The Sydell and Arnold Miller Family Heart & Vascular Institute Resource Nurses can answer your questions about PDA in older children and adults and help you make an appointment with a Cleveland Clinic adult congenital heart specialist.
Suggested reading and references
- Devanagondi R, Latson L, Bradley-Skelton S, Prieto L. Results of Coil Closure of Patent Ductus Arteriosus Using a Tapered Tip Catheter for Enhanced Control. Catheter Cardiovasc Interv. 2016 Aug;88(2): 233-8. doi: 10.1002/ccd.26415. Epub 2016 Jan 23.
- Gurcun U, Boga M, Badak M, et al. Transpulmonary Surgical Closure of Patent Ductus Arteriosus with Hypothermic Circulatory Arrest in an Adult Patient. Texas Heart Inst J. 2005;32(1):88-91.
- Krasuski R, Patent Ductus Arteriosus Closure. J Interven Cardiol. 2006;19:S60–S66.
- Prieto LR, DeCamillo DM, Konrad DJ, Scalet-Longworth L, Latson LA. Comparison of cost and clinical outcome between transcatheter coil occlusion and surgical closure of isolated patent ductus arteriosus. Pediatrics. 1998 Jun;101(6):1020-4.
- Prieto LR, Latson LA, Dalvi B, Arbetman MM, Ebeid MR, Lamorgese TT. Transcatheter coil embolization of abnormal vascular connections using a new type of delivery catheter for enhanced control. Am J Cardiol. 1999 Mar 15;83(6):981-3, A10.
Useful websites
- Patent Ductus Arteriosus, American Heart Association, www.heart.org.
- Canadian Adult Congenital Heart Network, www.cachnet.org.
- National Heart, Lung and Blood Institute, www.nhlbi.nih.gov/health-topics/patent-ductus-arteriosus.
- UpToDate, www.uptodate.com/contents/table-of-contents/patient-education.