What is amyloidosis?
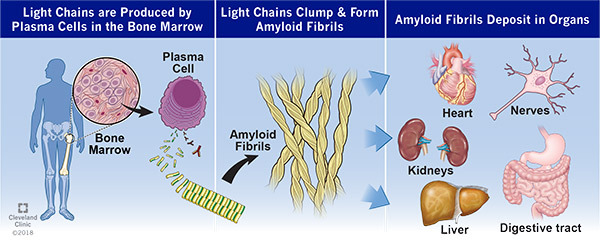
Amyloidosis (am-uh-loy-doh-sis) is a protein disorder. In this disease, proteins change shape (misfold), then stick together and form amyloid fibrils that are deposited in organs. As amyloid fibrils build up, the tissues and organs may not work as well as they should.
Our bodies make several proteins that can cause amyloidosis. To choose the right treatment, it is very important to know the exact protein that is causing the disease. The two most common types are light chain (AL) and transthyretin (ATTR) amyloidosis.
What is AL amyloidosis?
Light chains are pieces of antibodies made by white blood cells, specifically plasma cells, in the bone marrow. In AL amyloidosis, a group of plasma cells make too many light chains, which misfold and stick together to form amyloid fibrils. The fibrils are then deposited in organs. The most common organs affected are the heart and kidneys. Light chain amyloidosis can also affect the stomach, large intestine, liver, nerves and skin. The condition can cause problems with one or more parts of the body.
How is AL amyloidosis diagnosed?
Many tests can help diagnose amyloidosis. A biopsy (the removal of a small piece of tissue) of the affected organ(s) is the most useful test. A pathologist will examine the tissue under a microscope and perform special tests to identify the exact protein that is causing the amyloidosis.
Your doctor will talk to you about the biopsy/biopsies you need, which may include:
- Bone marrow biopsy: A small sample of bone marrow is removed from inside the bone. All patients with AL amyloidosis need a bone marrow biopsy.
- Kidney biopsy: An ultrasound is used to help guide a needle into the kidney. A few small pieces of tissue are removed.
- Heart biopsy: A small, thin, hollow tube (catheter) is guided to the heart through a vein in your neck. A few small pieces of the heart muscle are removed.
- Fat pad biopsy: A small piece of fat tissue is removed from your abdomen.
In addition to a biopsy, you may need other tests to find out how well your organs are working:
- Blood tests to check your kidneys, heart, liver and the amount of light chains in your blood.
- A 24-hour urine collection (done at home and returned to your doctor) to see if your kidneys are affected.
- Electrocardiogram (EKG) and echocardiogram (ultrasound of your heart).
- A cardiac MRI or a cardiac nuclear scan (technetium pyrophosphate scan) to see if your heart is affected.
Glossary of Terms
- Amyloid fibril: A rigid stack of amyloid proteins that builds up in organs.
- Amyloidosis: A disease caused by a buildup of abnormally shaped proteins (amyloid proteins) in organs.
- Stem cell transplant: A process in which the cells that make blood (stem cells) are removed before chemotherapy and replaced after treatment.
- Biopsy: A small piece of tissue that is removed and examined under a microscope.
- Cardiac magnetic resonance imaging (MRI): A scan that creates detailed pictures of the heart and shows how well it is working.
- Chemotherapy: Medications used to get rid of abnormal cells. Chemotherapy can include one or more medications.
- Echocardiogram: An ultrasound of the heart to show how well the heart is working.
- Electrocardiography (EKG): A recording of the heart’s electrical activity.
- Light chain: A piece of an antibody protein that is made by plasma cells in the bone marrow.
- Proteins: Large molecules that control the structure and function of the body’s tissues and organs.
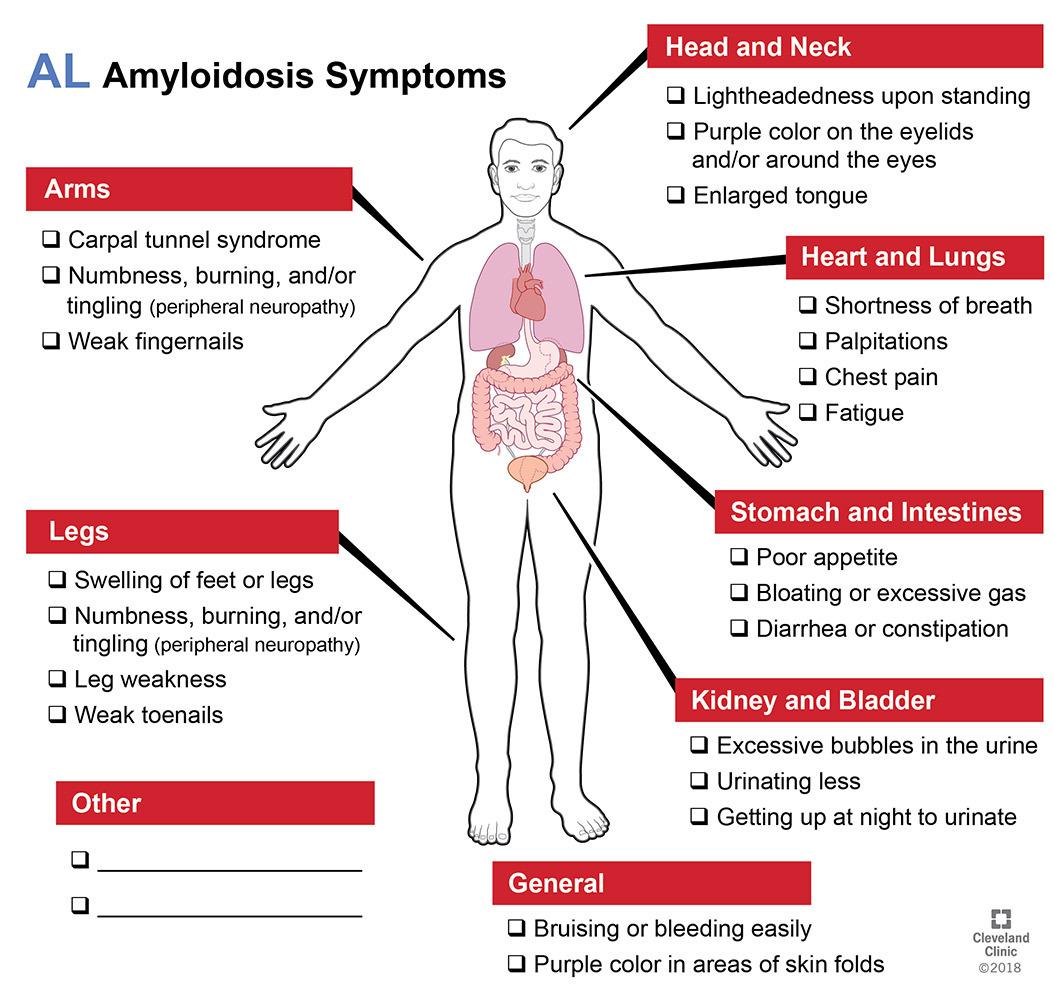
What are the symptoms of AL amyloidosis?
AL amyloidosis can affect many organs, and cause the following signs and symptoms:
What treatments are available for patients with AL amyloidosis?
A doctor who specializes in blood disorders (hematologist) will create a treatment plan for you.
Treatments for patients with AL amyloidosis include various medications:
Chemotherapy drugs
- Daratumumab (Darzalex).
- Cyclophosphamide (Cytoxan).
- Bortezomib (Velcade).
- Lenalidomide (Revlimid).
Steroid medications
- Dexamethasone.
- Prednisone.
Most patients take one or two chemotherapy drugs plus steroid medication. The drugs work together to destroy the plasma cells that make the light chain proteins. Your doctor may also talk to you about whether you may benefit from a bone marrow/stem cell transplant.
Medications can stop or slow the progression of AL amyloidosis but cannot remove the fibrils already in the body. A monoclonal antibody called CAEL-101 is being tested in clinical trials. It may be able to remove amyloid deposits in the affected organs.
Your treatment team will likely include:
- Cardiologist: A doctor that specializes in the heart.
- Gastroenterologist: A doctor who specializes in the gastrointestinal tract.
- Hematologist: A doctor that specializes in blood problems.
- Nephrologist: A doctor that specializes in the kidneys.
- Neurologist: A doctor that specializes in the nerves.
How does AL amyloidosis affect my life?
Amyloidosis is a long-term (chronic) disease that can be controlled. Early diagnosis and treatment are the keys to managing the disease before it becomes advanced.
Resources
- Cleveland Clinic Amyloidosis Center, clevelandclinic.org/amyloidosiscenter.
- Amyloid Foundation, amyloidosis.org, 877.269.5643 (1.877.AMYLOID), Email: info@amyloidosis.org.
- Amyloidosis Support Groups, amyloidosissupport.org, 1.866.404.7539, Email: info@amyloidosissupport.org.
- Amyloidosis Research Consortium, arci.org, 617.467.5170, Email: arc@arci.org.