What is a pacemaker?
A pacemaker is a device used to monitor your heart rate, keep it from going too slow and improve the coordination of your heart rhythm. A pacemaker has two main purposes:
- Sensing: Monitors your heart rate and rhythm.
- Pacing: Sends electricity to your heart if your heart rate is too slow or the rhythm is interrupted.
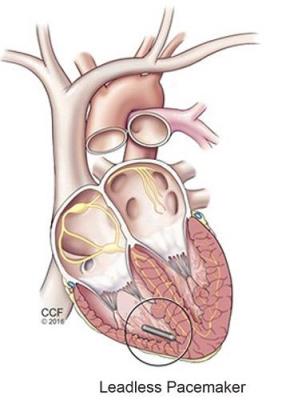
What is a leadless pacemaker?
A traditional pacemaker has wires (leads) attached to it. The leads go from the pacemaker, through your skin to your heart. They carry electrical impulses from the pacemaker to your heart to correct your heartbeat.
A leadless pacemaker does not use leads. It is a self-contained device that is implanted directly in your heart.
Can I have a leadless pacemaker instead of a traditional pacemaker?
You may be able to get a leadless pacemaker if you meet certain requirements, such as having a slow heart rate (bradycardia). A pacemaker (leadless or traditional) is not the best option for all patients. Your doctor can talk to you about your treatment options and testing to find out if a leadless pacemaker is a good treatment option for you.
Information About the Leadless Pacemaker Implant Procedure
How do I get ready for the procedure?
Driving
- Please arrange to have someone drive you home from the hospital. You will not be able to drive for 24 hours after the procedure.
Eating and Drinking
- You can eat a normal meal the night before your procedure, but do not eat or drink anything, including gum and mints, after midnight before your procedure.
- Do not swallow any water when you brush your teeth on the morning of your procedure.
Medicine
- Follow the instructions you get from your doctor or procedure scheduler about taking your medicine before your procedure. If you have any questions about what you should or should not take, call your doctor.
- If you need to take medicine the morning of your procedure, take it with only small sips of water.
- Bring a one-day supply of your medicine to the hospital. This is in case there is a change in your procedure time and you need to take medicine. DO NOT take any of this medicine without asking your doctor or nurse.
Clothing and Personal Items
- Dress in comfortable clothes that are easy to fold. You will wear a hospital gown for the procedure.
- Do not wear any make-up or nail polish.
- Do not wear jewelry or bring anything valuable with you to the hospital.
- You can bring a robe and toiletries. The person that comes to the hospital with you will hold onto these items until after your procedure.
What happens during the procedure?
Safety
- Your procedure team will verify your name, date of birth and procedure you are having.
- Your procedure team will cover you with sterile paper sheets (drapes), remove hair (if needed) and use a special cleanser on your body to prevent infection.
- You will have a soft strap over your waist and arms to keep you from touching the sterile area.
- You will get an IV to give you medicine, including an antibiotic to prevent infection.
- Your healthcare team will keep a close eye on your heart rhythm, blood pressure and blood oxygen level during the procedure.
Please let your procedure team know if you have any questions or concerns.
Pain management
- You will get medicine through your IV to make you drowsy and comfortable, but you will not get anesthesia to put you to sleep for the procedure.
- You will get local anesthesia at the incision site. You may feel a burning or pinching sensation when the medicine is injected. This quickly fades and the area will be numb.
- You may find it helpful to listen to music, guided imagery or another audio program during the procedure to help you relax and stay comfortable.
Please let the procedure team know if you feel any pain or discomfort during the procedure.
Putting the pacemaker in place
- Your doctor will make a small incision in your groin.
- A long, thin tube called a catheter is guided through the incision, into your femoral vein, and to your heart. Your doctor uses an X-ray machine to watch the catheter at all times.
- The pacemaker is put in place in your heart through the catheter.
- Your doctor will test the pacemaker. You may feel your heart beat faster, but you should not feel pain. If you do, tell your doctor.
- The catheter is removed, and the incision is closed using pressure and, often, a temporary suture. The suture is removed within 24 hours. You will have a bandage over the area to prevent infection.
- The procedure takes an hour, but the time can vary based on your individual needs.
What happens after the procedure?
You will either go home the same day or spend the night in the hospital. While you are in the hospital:
- You will lie flat and keep your leg straight for 2 to 6 hours after the procedure. This is to control bleeding.
- We will keep track of your heart rate and rhythm with a type of portable EKG monitor (telemetry monitor). The information from the monitor is displayed at the nursing station.
- You will have a chest X-ray to make sure the pacemaker is in the right place and go to the device clinic to make sure the pacemaker settings are correct.
- We will give you information about follow-up appointments, activity restrictions and signs of problems to look for after you go home.
- Please talk to your doctor about the medicine you need to take after your procedure. You may not need to take the same types or amounts of medicine that you took before you got your pacemaker.
- You will get a card with information about your pacemaker. This is a temporary card. You will get a permanent card in the mail within a few months of your procedure. Always carry the card with you.
Pacemakers and Electronics
Can I have an MRI?
Patients with a leadless pacemaker can usually have an MRI. Ask your doctor if it is safe for you to have an MRI. Before your scan, tell the MRI team that you have a pacemaker and the kind you have.
Can I use a cell phone and other electronics?
Some electronic devices use magnets that can affect the way your pacemaker works. To be safe:
- Do not use cell phones or smart watches on the side of your body your pacemaker is implanted.
- Do not carry your cell phone or other electronic devices in your shirt or coat pocket.
- Keep electronic devices at least six inches away from your pacemaker.
- Call your doctor if you notice any new signs or symptoms.