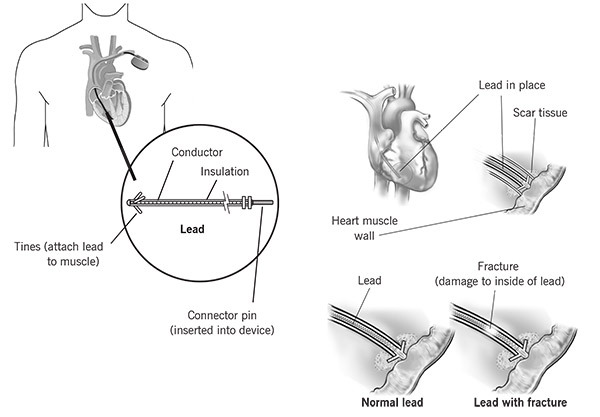
What is a lead?
A lead is a special wire that delivers energy from a pacemaker or implantable cardioverter defibrillator (ICD) to the heart muscle.
What is a transvenous lead extraction?
A transvenous lead extraction is the removal of one or more leads from inside the heart. Leads that are placed outside the heart during open heart surgery cannot be removed during this procedure.
Why do I need a transvenous lead extraction?
You need to have your lead(s) removed because you have one or more of these problems:
- Damage to the lead.
- Inefficient lead (needs too much energy or other issue).
- An infection near the device and/or lead.
- A clot or scar tissue that is causing a blockage in a vein.
How is the lead extraction performed?
There are two ways to extract leads:
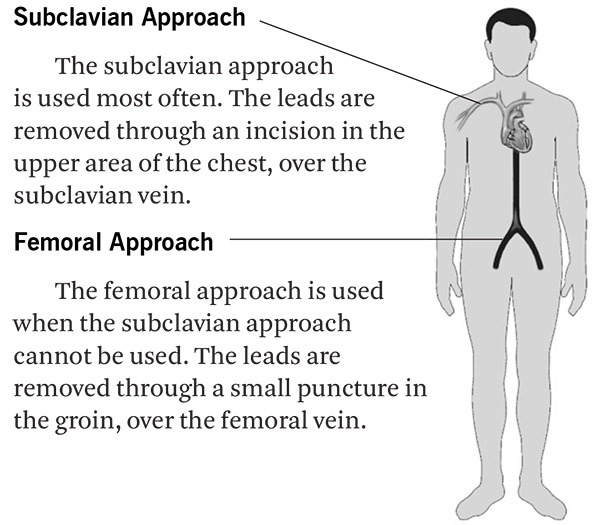
Removal of the lead
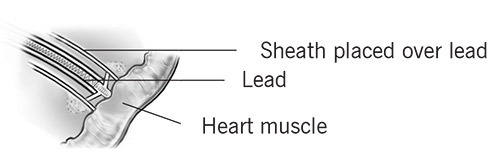
A tube (sheath) is placed in the vein. The sheath is threaded over the lead and guided to the tip of the lead (where the lead attaches to the heart).
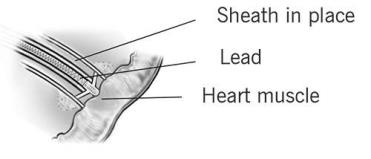
A laser light or mechanical drill-like tip can often be attached to the sheath to help break up the scar tissue.
The lead is then removed.
Are there risks to having a lead extraction?
A lead extraction is generally a very safe procedure. But, there are risks with all invasive procedures. Risks and results vary from patient to patient. Your doctor will talk to you about your risks and do everything possible to decrease them.
The overall clinical success rate for lead extraction over the last 10 years at Cleveland Clinic is greater than 97.8%. The risk of internal bleeding, tear in a vein or heart, or death is less than 1.7%.
Before the Procedure
What time will the procedure take place?
Call 800.223.2273 between the hours of 3:00 p.m. and 5:00 p.m. the day before your procedure and ask for the EP scheduling nurse, Pager 21215. If your procedure is scheduled on a Monday, call the Friday before. If your procedure is scheduled after a holiday, call the last business day before the holiday.
Should I take my medications?
You may need to stop taking some medications a few days before your procedure (such as blood thinners and aspirin). Do not stop taking any medication before asking your doctor.
If you must take medications before the procedure, swallow them with only small sips of water.
Can I eat?
Do not eat or drink anything after midnight the night before your procedure.
What happens before the procedure?
The procedure is done in a special surgical room. A nurse will help you get ready. You will put on a hospital gown. You may give your clothing to your family or keep it in a locker.
You will lie on a bed, and the nurse will start an intravenous (IV) line. This line is used to give you fluids and medications during the procedure. You will get an antibiotic through your IV to help prevent or treat infections.
You may need to have a transesophageal echocardiogram (TEE). A thin tube with a transducer goes into your throat after it is numbed. The transducer creates pictures of your heart.
You may have an arterial pressure line placed in an artery in your wrist or groin, and an IV will likely be placed in a vein in your groin. This is used to:
- Insert a pacemaker wire to keep your heart in rhythm when your pacemaker is removed.
- Insert tools used to remove the leads.
- Give you fluids, if needed.
- or for all of the above reasons if other veins are too.
If your doctor needs to access your groin, the area will be cleaned, draped and numbed. A needle is put in your vein in the same way an IV is started in your arm, only using a larger needle.
Once the line is in place, a catheter used to pace your heart will be inserted into the vein and guided to the right side of your heart. This is done only if your pacemaker/ICD is being replaced during the procedure. If you are getting a new pacing device at another time, the temporary pacemaker wires may be placed in your neck.
All catheters and temporary pacing equipment are usually removed at the end of the procedure, and the areas are covered with a bandage.
During the Procedure
To prevent infection or the spread of any infection you have, it is very important to keep the surgical areas sterile. Your chest and both sides of your groin will be shaved and cleansed with a special soap. Sterile drapes will cover you from your neck to your feet. As a reminder to keep your hands from coming into contact with the sterile drapes, soft restraints will be placed around your wrists, limiting the movement of your hands.
Will I be asleep?
General anesthesia is usually used so you "sleep" through the procedure. You may have a breathing tube.
If you do not get general anesthesia, you will get medication through your IV to make you drowsy. An anesthesiologist will be in the room during the procedure. If you are uncomfortable when you wake up, please tell the anesthesiologist.
You may feel pulling as the leads are removed, but you should not feel pain. Your doctor and nurse will be with you during the procedure. If you are uncomfortable or need anything, tell your nurse.
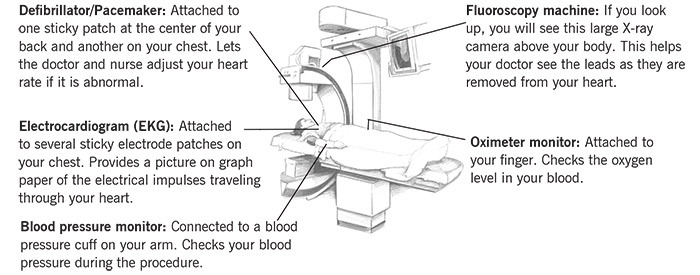
Several devices will be used to monitor your condition throughout the procedure.
Monitoring during the procedure
Will I get new leads?
New leads may be placed in your heart during this procedure or at a later date, depending on why the leads were removed. If they were removed because of an infection, you will be treated for the infection before you get new leads. If you have any questions or concerns about why your leads were removed or when they will be replaced, please ask your doctor.
Information About Fluoroscopic (X-ray)-Guided Procedures
During the lead extraction procedure, your doctor will use a fluoroscopy machine to see the leads as they are being removed.
Fluoroscopy uses X-rays to create a constant, moving picture to help guide small instruments through your blood vessels.
The X-ray beam is usually focused on a small patch of skin. This area of skin receives a higher dose of radiation than any other part of your body. Depending on the X-ray dose used, you may need to follow skin care instructions after the procedure.
You may have a mild to moderate sunburn-type skin reaction on the skin that received the most radiation. The skin reaction may take several days or weeks to develop. In extremely rare cases when very high doses of radiation are used, hair loss and skin damage are possible.
Before the procedure, please tell your doctor or nurse if you have ever had a fluoroscopy procedure, and whether you had any skin reaction.
If you have any questions or concerns about fluoroscopy, please discuss them with your doctor during your pre-procedure evaluation.
After the Procedure
How long will I stay in the hospital?
The lead extraction procedure takes 2 to 6 hours. Afterwards, you will stay in the hospital for 1 to 10 days.
If your leads were removed through your groin, you will need to lay flat in bed for several hours after the procedure.
If your new device and leads are implanted at the time your old leads are removed, you may be able to go home the morning after the extraction procedure.
If your device and leads are not replaced at the time of the extraction, you may need to stay in the hospital until they are implanted. Your doctor will tell you how long you should expect to be in the hospital and when your new device and leads will be implanted.
While you are in the hospital, your heart rate and rhythm are constantly monitored. This is done with a small box called a telemetry monitor. The box has wires that connect to your chest with electrode patches.
You may have stitches that will be removed 10 to 14 days after your procedure. Please ask your doctor about this.
If your leads were removed because of infection, you will likely get antibiotics after the procedure, either by mouth or through your IV. You may need to keep taking the antibiotics when you go home.
The morning after your procedure, you will have a chest X-ray to check your lungs and the position of any new leads that were implanted.
Follow-up care
Look at your incision(s) every day using a mirror. Call your doctor if you have:
- More swelling than usual near the incision or in your fingers or toes.
- More bleeding or drainage than usual.
- A temperature above 101 degrees F (38.6 C).
Before you leave the hospital, you will get information about activity limits, medications and follow-up appointments. If you have questions, please ask.
If you have any questions after you are home, call your doctor’s office M–F, 8:00 a.m.–5:00 p.m. After 5:00 p.m. and on weekends/holidays, call 888.490.6121 to talk to a registered nurse 24/7 or call 800.223.2273 and ask for the EP Fellow on call at Pager 20353.
Action Checklist
Before the procedure
Call 800.223.2273 between 3:00 p.m. and 5:00 p.m. the day before your procedure. Ask for the EP scheduling nurse. If your procedure is scheduled on a Monday, call the Friday before. If your procedure is scheduled after a holiday, call the last business day before the holiday.
- DO NOT eat or drink anything after midnight the night before your procedure.
- Ask your doctor about which medications you should and should not take before the procedure.
- DO NOT bring valuables to the hospital.
After the procedure
- You will stay in the hospital.
- Your doctor will talk to you about medications, activity limits and follow-up guidelines to follow at home.