What is fibromuscular dysplasia?
Fibromuscular dysplasia (FMD) is a rare medical condition. Patients with FMD have abnormal cellular growth in the walls of their medium and large arteries. This can cause the arteries with the abnormal growth to look beaded. The arteries may also become narrow (stenosis).
Most cases of FMD affect the carotid and renal arteries. The carotid arteries are in the neck and connect the heart and the brain. The renal arteries are the blood vessels that carry blood from the aorta to the kidneys.
Fibromuscular dysplasia can also affect the arteries to the intestines (the mesenteric arteries), the arteries to the legs or arms, the coronary arteries (arteries that supply blood to the heart), and arteries in other parts of the body, although this is less common. Many times, arteries in more than one location are affected by FMD.
Who is affected by FMD?
Fibromuscular dysplasia is most common in women between the ages of 40 and 60, but the condition can also occur in children and the elderly. The majority (more than 90%) of patients with FMD are women. However, men can also have FMD, and those who do have a higher risk of complications such as aneurysms (bulging) or dissections (tears) in the arteries.
What causes FMD?
Despite a great deal of research, it is still not clear what causes FMD. It is very likely that FMD has multiple underlying causes. Some of the factors that may play a role include:
- Hormonal influences: The disease occurs most commonly in women.
- Genetics: About 7-11% of cases are inherited. Some patients with FMD also have genetic abnormalities that affect the blood vessels.
- Internal mechanical stress, including trauma to the artery walls or mechanical forces on the vessel.
- Loss of oxygen supply to the blood vessel wall: This occurs when the tiny blood vessels in the artery walls that supply them with oxygen-rich blood gets blocked by fibrous lesions.
Types of fibromuscular dysplasia
Artery walls have three layers:
- Tunica Intima (the inside layer).
- Tunica Media (the middle layer).
- Adventitia (the outside layer).
In the past, FMD was classified according to the layer of the artery that was affected and by the lesions a patient had. There were five different types of FMD — medial fibroplasia, intimal fibroplasia, perimedial fibroplasia, medial hyperplasia, and periarterial hyperplasia. However, the only way to absolutely know which of these types of FMD a patient has is to look at the artery wall under a microscope, such as after a biopsy or surgical procedure, and this is rarely done. The majority of patients with FMD are diagnosed using imaging studies, such as angiography. As a result, the types of FMD were recently simplified to match the appearance of FMD in these studies. The condition is now classified as either multifocal or focal FMD.
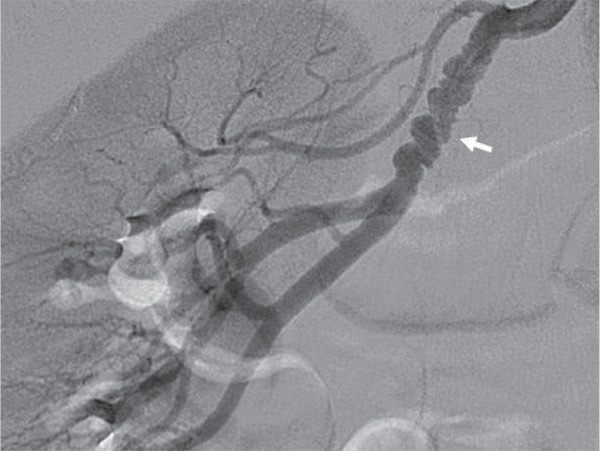
Figure 1: Fibromuscular dysplasia of the right renal artery. The classic "beads on a string" appearance is typical of medial fibroplasia, the most common type of FMD. In this case, there is mild to moderate narrowing of the artery.
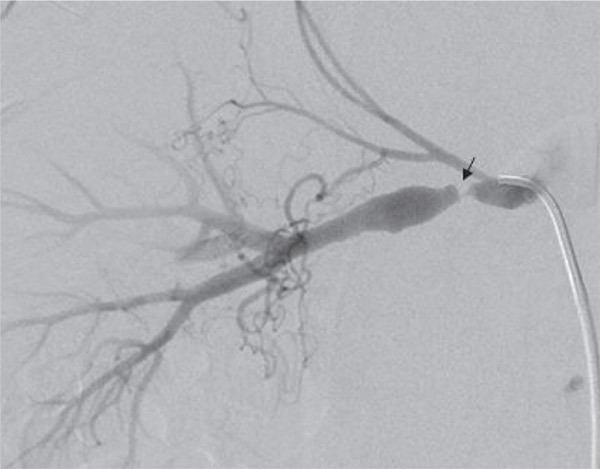
Figure 2: Fibromuscular dysplasia of the right renal artery. The smooth, concentric narrowing (arrow) has the typical appearance of intimal fibroplasia. In this case, there is severe narrowing of the artery, and the patient was treated with balloon angioplasty.
Multifocal FMD
- Affects approximately 90% of patients with FMD.
- Patients have multiple lesions; most often appears as a "string of beads," which is caused by alternating areas of widening and narrowing along the artery.
- Includes medial fibroplasia and perimedial fibroplasia types of FMD.
- Medial fibroplasia is the most common type of FMD in this category.
Focal FMD
- Affects less than 10% of patients with FMD.
- Patients have distinct focal lesions or tubular narrowing (stenosis).
- Includes intimal fibroplasia, periarterial fibroplasia, and medial hyperplasia types of FMD.
- Intimal fibroplasia is the most common type of FMD in this category.
What are the symptoms of FMD?
Some people with FMD do not have any symptoms, but symptoms can occur if the stenosis restricts blood flow through the affected artery.
Symptoms of FMD in the carotid or vertebral arteries (that supply blood to the back of the brain) may include headaches (especially migraine-type headaches), a pulsatile "swooshing" noise in the ears, neck pain and lightheadedness. If FMD affects the carotid arteries, the doctor will hear a swooshing nose in the back of the neck. This is called a bruit and means there is abnormal blood flow to the area. More advanced cases of FMD can cause a transient ischemic attack (TIA) or stroke.
FMD of the carotid or vertebral arteries can lead to a tear in the artery. This is called a dissection. Symptoms of dissection include headache, sudden neck pain, drooping of one of the eyes or unequal pupils, and, in severe cases, symptoms of stroke or TIA.
FMD of the renal arteries frequently causes high blood pressure in these arteries (renovascular hypertension) and/or poor kidney function (renal insufficiency). FMD usually does not lead to kidney failure.
FMD of the mesenteric arteries (arteries to the intestines) may cause abdominal pain after eating and weight loss, but patients may not have any symptoms.
FMD of the extremities may cause pain in the affected area during exercise (claudication), or much less commonly, acute limb ischemia.
FMD of the coronary arteries has recently been associated with spontaneous coronary artery dissection (SCAD). Coronary artery dissection usually causes chest pain and heart attack.
How is FMD diagnosed?
Sometimes, patients are diagnosed with FMD after having an X-ray or scan for another problem, and the doctor sees the beaded appearance of the arteries.
Some patients are diagnosed with FMD during a routine exam after the doctor hears a swooshing noise, called a bruit, which means there is abnormal blood flow.
Once FMD is discovered in one part of the body, more imaging tests are usually done to check for FMD in other areas. For example, if you have carotid FMD and high blood pressure, you might have a test to check for FMD in your renal arteries.
You may need more tests, such as a duplex ultrasound (or Doppler), magnetic resonance angiography (MRA) or computed tomography angiography (CTA). These noninvasive tests can be used to confirm the diagnosis of FMD and determine the extent of the lesions.
Your doctor may also recommend a dye angiogram. This is considered the gold standard for diagnosing FMD. In general, dye angiogram studies are done only if the diagnosis of FMD is not clear, or if you need a procedure such as a balloon angioplasty, which can be done at the same time.
If you are diagnosed with FMD, you should have tests to check for an aneurysm (in the brain or aorta/aortic branches) that may require additional treatment.
What treatments are available for patients with FMD?
There are several treatments available for patients with FMD. Your doctor will talk to you about the type of treatment that is best for you, based on the type of FMD you have, how severe your condition is, and your overall health.
Medications
If you have FMD but do not have any symptoms, you likely won’t need an interventional treatment. Your doctor may prescribe an antiplatelet medication (prescription medication or aspirin) to prevent blood clots.
If you have high blood pressure in your renal arteries (renovascular hypertension) as a result of FMD, you may need to take medication to control your blood pressure. Common medications include angiotensin converting enzyme inhibitors (ACE-inhibitors) and angiotensin receptor blockers (ARBs).
If you have FMD and have frequent headaches, especially migraine headaches, your doctor may prescribe medication as treatment or prevention. If your headaches are severe and frequent, you may need to see a doctor who specializes in treating patients with headaches.
Identify and Treat Risk Factors
High blood pressure, diabetes and high cholesterol are all risk factors for vascular disease. It is important to be checked for these conditions and follow your treatment plan. It is also important not to smoke.
You may need to have regular testing, such as a duplex ultrasound, MRA or CTA, to monitor your condition. Testing is usually done once a year. These regular checks are especially important if you have an aneurysm or a carotid, vertebral, or renal artery dissection.
Angioplasty
Your doctor may recommend that you have percutaneous angioplasty of the renal arteries. This procedure is similar to the procedure used to treat patients with blockages in the coronary arteries. A long, thin tube called a catheter with a tiny balloon on the end is inserted into the artery and guided to the narrowed/blocked area with the help of a special X-ray machine. Then, the balloon is inflated, which causes the blood vessel to re-open, and then the balloon and the catheter are removed.
Although it is common for patients who have angioplasty for heart-related problems to have a stent (small, metal mesh tube) placed in the area that is unblocked, there is no proof that stents improve outcomes related to renal angioplasty. In general, renal artery stents should only be used if angioplasty alone doesn’t restore proper blood flow to the kidneys or if they are needed to treat patients with a dissection (tear) in the renal artery.
Angioplasty may be recommended for patients with FMD of the internal carotid artery who have TIAs or stroke due to severe narrowing of the arteries. Stenting may also be needed in rare cases, such as when patients with FMD have had carotid or vertebral artery dissection that has not healed despite treatment with medication or who have a carotid aneurysm.
Surgery
Your doctor may recommend reconstructive surgery if you have complex FMD of the renal arteries, depending on how severe the disease is and the areas affected. Surgery generally involves restoring blood flow by removing the blocked section of the artery or creating a bypass around the blockage. Surgery may also be the best option for patients who have an aneurysm but cannot be treated using catheter-based techniques.
FMD is a very different disorder than atherosclerosis (the build-up of plaque that is the most common cause of blocked arteries). Angioplasty and reconstructive surgery are technically demanding procedures and should be performed only by a physician experienced in these procedures and in the care of patients with FMD.
Resources
- Fibromuscular Dysplasia Society of America (a website dedicated to building awareness of FMD, funding research activities, providing patient support, and educating patients and the healthcare community.)
- Whooshers (www.wooshers.com online forum and information center for sufferers of pulsatile tinnitus and the medical professionals dedicated to treating them.)
Additional resources and references are available at: http://my.clevelandclinic.org/services/heart/disorders/fibromuscular_dysplasia.
FMD clinic
Cleveland Clinic provides specialized care for patients with fibromuscular dysplasia in the FMD Clinic. Care is provided by vascular medicine specialists who collaborate with a multidisciplinary team, including interventional cardiologists, vascular surgeons, nephrologists, neurologists, radiologists and geneticists. Your healthcare team will work with you to develop a treatment plan tailored to your needs and condition.