What is an implanted loop recorder?
An implanted loop recorder is a heart monitor that is surgically implanted. The device is about the size of a pen cap. It helps your doctor understand your condition and the cause of symptoms such as unexplained fainting (syncope), palpitations and abnormal heart rhythms (arrhythmias). An implanted loop recorder can be used to collect information about your heart rhythm for up to 36 months.
Who needs an implanted loop recorder?
An implanted loop recorder may be recommended for people who:
- Have an increased risk of abnormal heart rhythms (arrhythmias).
- Have repeat episodes of brief, spontaneous symptoms that might be caused by an arrhythmia.
- Need long-term monitoring to capture arrhythmias that may be hard to detect with other methods.
- Your doctor will talk to you about whether a loop recorder is right for you.
How does the implanted loop recorder work?
The implanted loop recorder constantly monitors and records your heart rate and rhythm. When you have symptoms, you will place a hand-held activator over the monitor and press a button. The recorder captures information about your heart’s electrical activity for a set amount of time before you press the button.
If you faint, the recorder can be activated when you wake up, or another person can use the activator to capture the information. It is important to keep the activator with you at all times.
Your doctor will also program the device to automatically record your heart’s electrical activity, even when you do not have symptoms. Auto-activation mode may detect episodes that do not cause symptoms, including:
- Asystolic pauses (brief stopping of the heart).
- Bradycardia (slow heart rate).
- Tachycardia (fast heart rate).
Your cardiologist will review the stored information during your follow-up appointment.
The device can be removed after it has recorded an episode of arrhythmia or when your doctor has enough information to evaluate your condition.
Is the loop recorder implant procedure safe?
The loop recorder implant procedure is an outpatient procedure done using a minimally invasive technique. It is generally very safe; however, all procedures have risks. Specific risks include infection at the implant site and an allergic reaction to the local anesthetic. Special precautions are taken to decrease these risks. Please talk to your doctor about any concerns you have, as well as the risks and benefits of the procedure.
Before the Procedure
Where is the implant procedure done?
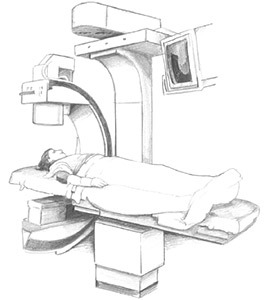
The implant procedure takes place in a specialized room in the Electrophysiology Lab.
Should I take my medications?
- Ask your doctor if you need to stop taking any medications before the procedure and when you should stop taking them.
Do not stop taking any of your medications unless your doctor tells you to.
- If you have diabetes, ask the nurse about changes you need to make to your diabetes medications or insulin.
Can I eat before the procedure?
- Eat a normal meal the evening before your procedure.
- DO NOT eat, drink or chew anything after 12 midnight before your procedure. This includes gum, mints, water, etc.
- If you need to take medications, take them with only small sips of water. Do not swallow any water when you brush your teeth.
What should I wear?
Cosmetics
- Please do not wear makeup or nail polish.
- Wear comfortable clothes. You will wear a hospital gown for the procedure.
- Leave all jewelry (including wedding rings), watches and other valuables at home.
What should I bring?
- A responsible adult driver must come with you to the hospital and drive you home after the procedure. The sedative used during the procedure may make it unsafe for you to drive or operate machinery.
- Bring a one-day supply of your prescription medications. Do not take these medications without first talking with the doctor or nurse.
- You may find it helpful to listen to music or guided imagery.
- You may want to bring a book, cards or puzzles to pass the time while you wait.
What happens before the procedure?
- The nurse will start an IV (intravenous) line in a vein in your arm or hand. The IV is used to give you medications and fluids during the procedure.
- To prevent infection and to keep the device insertion site sterile: You will get an antibiotic through the IV at the beginning of the procedure. The left or right side of your chest will be shaved, if needed.
- The area will be cleansed with a special soap.
- You will be covered with sterile drapes.
- A soft strap may be placed across your waist and arms to keep you from touching the sterile area.
During the Procedure
Will I be awake?
You will get a sedative to relax you and make you feel drowsy, but you will be awake during the procedure.
How will I be monitored?
Several monitors are used to constantly check your heart rhythm and blood pressure during the procedure.
How is the loop recorder implanted?
The first step is to numb the area. Then, a small (about 1/4-inch) incision is made in the skin on your upper chest. The loop recorder is placed under the skin through this incision. The incision will be closed with either skin glue or stitches that will dissolve in a few days.
What will I feel?
You will feel a burning or pinching sensation when the doctor gives you the anesthetic. The area will quickly become numb. You may feel a pulling sensation as the doctor places the loop recorder under the skin. Tell your doctor if you feel anything. You should not feel pain. If you do, tell your nurse right away.
Will the loop recorder change my physical appearance?
You may have a small scar after the incision has healed. There will be a slightly elevated area on the skin where the device is implanted.
How long does the procedure last?
The procedure itself lasts about 20 to 30 minutes, but the preparation and recovery time add several hours. Please plan to stay at Cleveland Clinic for 4 to 6 hours.
Will I have to stay in the hospital?
You will likely go home the same day as the procedure. A bandage will be placed over the device insertion site, and you will go to a short-stay recovery room until you go home. You must have a responsible adult driver to take you home.
Identification card
You will get an identification (ID) card that lists:
- The type of loop recorder you have.
- The device manufacturer.
- The date of the implant procedure.
- Your doctor’s name.
It is important to carry this card at all times in case you need medical attention.
After the Procedure
How do I take care of my incision?
- Remove the bandage the day after the procedure.
- A small amount of bruising or swelling is normal.
- Do not shower for 5 days after the procedure.
- Check the incision site every day for signs of infection (redness, swelling or drainage).
Follow-up instructions
- We will teach you how to use the activator to record symptoms. Please let us know if you have any questions.
- Your doctor will tell you which medications you need to take after the procedure.
Monitoring and transmissions
Remote monitoring
Remote monitoring is wireless after it is set-up. Data is automatically sent to your clinic once a month. You can send information in between your scheduled send dates by using the activator.
If you can use remote monitoring, you will get detailed instructions on how to send transmissions. The equipment will be sent to your home, and you will be automatically enrolled in the program.
Monitors used during the procedure
Defibrillator/pacemaker/cardioverter: Attached to one sticky patch placed on the center of your back and one on your chest. This is used to adjust your heart rate if it is too fast or slow during the procedure.
Electrocardiogram (ECG/EKG): Attached to several sticky electrode patches placed on your chest, as well as inside your heart. Creates a picture of the electrical impulses traveling through the heart.
Blood pressure monitor: Connected to a blood pressure cuff on your arm. Checks your blood pressure throughout the procedure.
Oximeter monitor: Attached to a small clip placed on your finger. Checks the oxygen level of your blood.
Follow up visits and questions
In-person follow-up
If you cannot use remote monitoring, you will have follow-up appointments in the Device Clinic every 3 months.
When should I call the doctor?
Call your doctor right away if you have any signs of infection, such as:
- Increase in drainage, bleeding or oozing from the insertion site.
- Opening of the incision.
- Redness or warmth around the incision.
- A fever - temperature higher than 101 degrees Fahrenheit or 38.4 degrees Celsius.
- If you have any questions or concerns.
How long does the recorder stay in place?
The recorder stays in place until your doctor has more information about your condition and can tell if you have an arrhythmia. The battery lasts about 3 years.