What is a cardiac arrhythmia?
A cardiac arrhythmia, also called dysrhythmia, is an irregular or abnormal heart rhythm.
What is catheter ablation?
Catheter ablation is a treatment for cardiac arrhythmias. During ablation, a doctor inserts a catheter (thin, flexible tube) into the heart. A special machine delivers energy through the catheter to tiny areas of the heart muscle that cause the abnormal heart rhythm. This energy “disconnects” the pathway of the abnormal rhythm. Ablation can also be used to disconnect the electrical pathway between the upper chambers (atria) and lower chambers (ventricles) of the heart. The type of ablation performed depends upon the type of arrhythmia.
What types of rhythms are treated with this procedure?
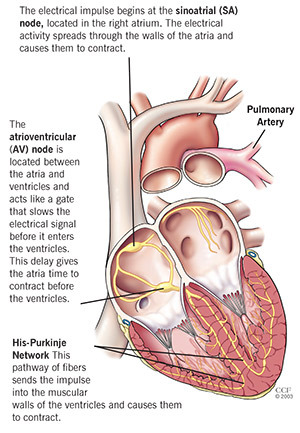
Normally, the heart’s impulses travel down an electrical pathway through the heart. The atria and ventricles work together, alternately contracting and relaxing to pump blood through the heart. The electrical system of the heart is the power source that makes this possible. Each electrical impulse causes the heart to beat. Catheter ablation can be used to treat:
- AV Nodal Reentrant Tachycardia (AVNRT): An extra pathway lies in or near the AV node, which causes the impulses to move in a circle and re-enter areas it already passed through.
- Accessory Pathway: Extra pathways can exist from birth that connect the atrium and ventricles. The extra pathway causes signals to travel back to the atrium, making it beat faster.
- Atrial Fibrillation and Atrial Flutter: Extra signals that start in different parts of the atrium cause the atria to beat too fast (atrial flutter) or quiver (atrial fibrillation).
- Ventricular tachycardia: A rapid, potentially life-threatening rhythm that starts in the ventricles. The rapid rate keeps the heart from filling with enough blood, and less blood is able to move through the body.
How successful is catheter ablation?
The success rate depends on your individual health and the type of catheter ablation you have. Talk to your doctor about the success you can expect.
Are there any risks?
The catheter ablation procedure is generally very safe. However, there are risks with any procedure. Special precautions are taken to decrease these risks. Your doctor will discuss the risks of the procedure.
Evaluation
A thorough evaluation is needed to determine if catheter ablation is an appropriate treatment option for you. This evaluation may include:
- A review of your medical history.
- Complete physical examination.
- Electrocardiogram (ECG).
- Echocardiogram (Echo).
- Holter monitor test.
- Other tests as needed.
After the evaluation, your doctor will talk to you about your treatment options and, together, you will decide the best option for you.
Before the Procedure
Should I take my medications?
Please call your doctor’s office one week before your procedure to find out if you need to stop taking any of your regular medications.
DO NOT stop taking any of your medications without first talking to your healthcare provider. If you have diabetes, ask the nurse how you should adjust your diabetes medications and/or insulin.
Can I eat before the procedure?
Eat a normal meal the evening before your procedure. DO NOT eat, drink or chew anything after 12 midnight before your procedure. This includes gum, mints, water, etc. If you need to take medications, take them with small sips of water. Do not swallow any water when you brush your teeth.
What should I wear?
Wear comfortable clothes. You will change into a hospital gown before the procedure. Please leave all jewelry (including wedding rings and watches) and other valuables at home.
The clothes you wear that morning will be returned to the person who accompanies you or placed in a locker.
Remove all makeup and nail polish before you come to the hospital.
What should I bring?
You will not need a robe or toiletries when you first arrive. Your family member can keep these items to give you after the procedure. Bring your prescription medications with you, but do not take them without first talking to your healthcare provider.
You may bring guided imagery materials or music to listen to before the procedure (don’t forget to bring your audio player!).
What happens when I arrive?
You will lie on a bed, and the nurse will start an intravenous line (IV) in your arm. The IV is used to deliver medications and fluids during the procedure.
You will get medication through your IV to make you feel drowsy. You may fall asleep.
Your neck, upper chest, arm and groin will be cleansed with an antiseptic solution, and the catheter insertion site(s) will be shaved. Sterile drapes will be placed to cover you from your neck to your feet.
During the Procedure
Where is the procedure performed?
The catheter ablation takes place in a special room called the electrophysiology (EP) lab.
Will I be monitored?
The nurse will connect you to several monitors that will constantly check your heart rhythm and your body’s responses to any arrhythmias you may have during the procedure.
How does the doctor insert the catheters?
After you are drowsy, the doctor will numb the catheter insertion site(s) with medication. The doctor will insert several catheters through a small incision into a large blood vessel (in your groin, neck or arm, depending on the type of ablation procedure being performed). It may be necessary to use both an artery and a vein. A transducer is inserted through one of the catheters to perform an ultrasound inside your heart during the procedure. The ultrasound lets the doctor see the structures of your heart.
The catheters are passed through the blood vessels to your heart. After the catheters are in place, the doctor looks at a monitor to check your heart’s conduction system. The doctor then uses a pacemaker-like device to send electrical impulses to the heart to increase your heart rate.
If your arrhythmia occurs during the procedure, you’ll be asked to describe the symptoms you feel.
The doctor uses the catheters to locate the area or areas where the arrhythmia starts. Once the area is located, energy is sent through the catheter to stop the abnormal impulses.
Once the ablation is complete, the electrophysiologist uses monitoring devices to observe the electrical signals in the heart to ensure that the abnormal rhythm was corrected.
What will I feel?
You will feel a burning sensation when the doctor injects medication into the catheter insertion site. You may feel your heart beating faster or stronger when the doctor uses the pacemaker device to increase your heart rate, and you may feel some discomfort or a burning sensation when the energy is applied.
It is important to remain quiet, keep very still and avoid taking deep breaths. If you feel pain, ask your doctor or nurse to give you more medication.
During the procedure, you will be asked to report any symptoms, answer questions or follow instructions from your doctor.
How long does the procedure last?
The procedure may last 4 to 8 hours.
Monitors Used During the Procedure
Defibrillator/pacemaker/cardioverter: Attached to one sticky patch placed on the center of your back and one on your chest. This lets the doctor and nurse pace your heart rate if it is slow, or send energy to your heart if the rate is too fast.
Electrocardiogram (EKG): Attached to several sticky electrode patches placed on your chest and inside your heart. Provides a picture on the monitors of the electrical impulses traveling through your heart.
Blood pressure monitor: Connected to a blood pressure cuff on your arm. Checks your blood pressure throughout the ablation.
Mapping system: State-of-the-art technology that helps your doctor find the exact area of your arrhythmia.
Oximeter monitor: Attached to a small clip placed on your finger. Checks the oxygen level in your blood.
Fluoroscopy: A large X-ray machine positioned above you to help the doctors see the catheters during the procedure.
Intracardiac ultrasound: Performed by a catheter inserted into the heart. Intracardiac ultrasound is used throughout the procedure to view the structures of the heart and the catheter when it is in contact with the heart lining.
After the Procedure
What should I expect after the procedure?
The doctor will remove the catheters and apply pressure to the insertion site to prevent bleeding. You will need to stay in bed for 1 to 6 hours after the procedure to prevent bleeding. You’ll need to keep your legs still during this time.
No stitches are needed. A small sterile bandage (dressing) will cover the insertion site. Keep this area clean and dry. Tell your doctor or nurse right away if you have redness, swelling or drainage at the procedure site. You can remove the bandage at home.
During your recovery, you will be placed on a telemetry monitor, which lets the nurses watch your heart rate and rhythm. Telemetry consists of a small box connected by wires to your chest with sticky electrode patches. The box displays your heart rhythm on several monitors in the nursing unit.
Will I have to stay in the hospital?
Some patients are sent home the same day, while others stay overnight in the hospital after the procedure. Your doctor will let you know what is best for you.
When will I find out the results?
After the procedure, the doctor will discuss the results of the procedure with you and your family and answer any questions you have.
How will I feel after the procedure?
You may feel fatigue or chest discomfort during the first 48 hours after the procedure. Please tell your doctor or nurse if any of these symptoms are prolonged or severe.
You may have skipped heartbeats or short episodes of atrial fibrillation after the procedure. These abnormal heartbeats should stop after your heart is healed.
What instructions will I get before I leave the hospital?
You will get specific instructions about how to care for yourself after the procedure, including medication guidelines, wound care, activity guidelines, pacemaker care and maintenance, and a follow-up schedule.
Will I need to take new medications?
You may need to take an antiarrhythmic medication to control abnormal heartbeats. Your doctor will give you the prescriptions and medication instructions you need. Ask your doctor if you should keep taking your previous medications.
Will I be able to drive myself home?
For your safety, a responsible adult must drive you home.
Action Checklist
Before the Procedure
- DO NOT stop taking any medication before you talk to your doctor (call 1 week before the procedure to get medication instructions).
- Do not eat or drink anything after midnight the night before the procedure.
- Do not bring jewelry or valuables to the hospital.
After the Procedure
- You may stay in the hospital overnight.
- Your doctor and nurse will talk to you about your procedure results, medications, homegoing instructions and follow-up schedule.
- If you have any questions, please ask.