What is cardiac resynchronization therapy?
Some patients with advanced heart failure have a problem with their heartbeat caused by delayed electrical activation in the lower chambers of the heart (ventricles). Cardiac resynchronization therapy (CRT) is used to fix this problem.
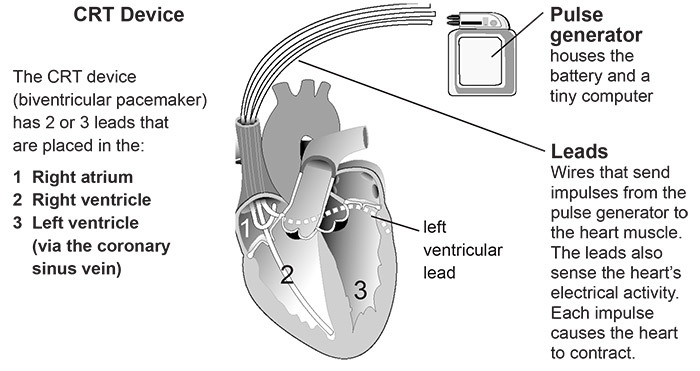
The CRT pacing device is also called a biventricular pacemaker. It is a battery-powered device that is placed under the skin during surgery. The device has two or three wires (leads) that are placed in the heart to help keep your heartbeat balanced. The leads are put in place through a vein in the upper right chamber of your heart (right atrium), right ventricle and into the coronary sinus vein.
How it works: Your doctor will program the device so that if your heart rate drops below a certain point, the device will send small electrical impulses through the leads to the heart muscle. This forces the ventricles to contract and causes the right and left ventricles to pump together, which helps your heart work better.
Heart failure means the heart’s pumping power is weaker than normal. Blood moves through the heart and body at a slower rate, causing more pressure in the heart. If you have heart failure, it is common for there to be too much time between the contractions of the right and left ventricles. This keeps the walls of the left ventricle from contracting at the same time.
Electrical system of the heart
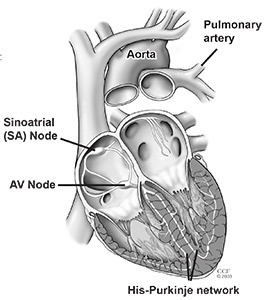
The atria and ventricles work together, taking turns contracting and relaxing to pump blood through the heart. The electrical system of the heart is the power source that makes this possible.
Normally, the electrical impulse starts at the sinoatrial (SA) node, which is in the right atrium. The electrical activity spreads through the walls of the atria, causing them to contract.
Next, the electrical impulse moves through the AV node, which is between the atria and ventricles. The AV node acts like a gate that slows the electrical signal before it enters the ventricles. This delay gives the atria time to contract before the ventricles do.
From the AV node, the electrical impulse travels through the His-Purkinje network. This is a pathway of specialized fibers that conduct electricity. Then the impulse moves into the muscular walls of the ventricles, causing them to contract. This sequence repeats every time your heart beats (usually 60–100 times per minute).
CRT and ICD therapy
Some patients with heart failure may benefit from a combination of CRT and an implantable cardiac defibrillator (ICD). The combination offers biventricular pacing plus anti-tachycardia pacing and internal defibrillation to deliver treatment as needed.
About 90 percent of Cleveland Clinic patients who receive a biventricular device receive one that also provides defibrillator therapy. However, only about 40 percent of the patients who receive defibrillators are also candidates for a device that includes biventricular stimulation (CRT/ICD combination device).
The information in this handout refers to CRT and ICD combination therapy.
The CRT/ICD combination device:
- Resynchronizes the heartbeat.
- Slows down an abnormal fast heart rhythm.
- Prevents abnormally slow heart rhythms.
- Records a history of the patient’s heart rate and rhythm.
Some CRT and ICD combination therapies have an internal monitoring device inside so your doctor or nurse can track your heart rhythm and heart function, such as the pressure in areas of your heart.
You may be asked to use a telephone to send data electronically from your device to a computer server so your doctor or nurse can monitor your condition.
Benefits of CRT
CRT improves symptoms of heart failure in about 65% of patients who still have moderately severe to severe symptoms even while taking the highest possible doses of medications. The therapy improves survival, quality of life, heart function, the ability to exercise, and helps decrease hospitalizations in select patients with severe or moderately severe heart failure.
Is the device implant procedure safe?
A device implant is generally a very safe procedure. But, all procedures involve risks. We take every precaution to reduce these risks. Please talk to your doctor about any questions or concerns you have.
Will CRT improve my ejection fraction?
Yes, CRT can help improve your ejection fraction. Ejection fraction (EF) is the measurement of how much blood is being pumped out of the left ventricle of the heart. A normal EF ranges from 50% to 70%.
People with heart failure who have a poor ejection fraction (EF less than 35%) are at risk for fast, irregular and sometimes life-threatening heart rhythms. The CRT/ICD combination device can help protect you against these dangerous, fast heart rhythms.
Success of CRT
Cleveland Clinic experience has shown that CRT improves patients’ ejection fraction by 5% to 10%. In some cases, patients with a CRT device develop normal ventricular function. Based on our experience, it is not rare for a patient to increase his or her ejection fraction over 40%.
Who is eligible for a CRT device?
CRT may be an appropriate treatment if you:
- Have severe or moderately severe heart failure symptoms.
- Take medications for heart failure treatment.
- Have delayed electrical activation of the heart (such as intraventricular conduction delay or bundle branch block).
- Have a history of heart attack or are at risk of having a heart attack.
Together, you and your doctor will decide if this treatment is right for you.
Before the Procedure
Action checklist
- Do not eat anything after midnight the night before the procedure.
- Talk to your doctor about the medications you should take before the procedure.
- Do not bring valuables.
Should I take my medications?
- Do not stop taking any medication without first talking to your doctor. Ask your doctor which medications you should stop taking and when to stop taking them.
- If you take Coumadin (warfarin), the results of your INR test (a blood test to check your blood’s clotting ability) must be within a certain range before you can have the procedure.
- You will likely need to stop taking anticoagulant medications, including aspirin or Coumadin (warfarin), a few days before the procedure.
- Your doctor may tell you to stop taking other medications.
- If you have diabetes, ask your nurse about changes you need to make to your diabetes medications or insulin.
Can I eat before the procedure?
Eat a normal meal the evening before your procedure. DO NOT eat, drink or chew anything after 12 midnight before your procedure. This includes gum, mints, water, etc.
If you need to take medications, swallow them with small sips of water. Do not swallow any water when you brush your teeth.
What should I wear?
- Remove all makeup and nail polish.
- Wear comfortable clothes. You will change into a hospital gown for the procedure.
- Leave all jewelry (including wedding rings), watches and valuables at home.
What should I bring?
Bring a one-day supply of your prescription medications. Do not take these medications without first talking with the doctor or nurse.
You may want to pack a robe and toiletries to use after the procedure.
You may want to bring an audio player to listen to guided imagery or music.
What happens before the procedure?
A nurse will help you get ready for the procedure. You will have an IV (intravenous line) in a vein in your arm or hand. The IV is used to give you medications and fluids during the procedure.
To prevent infection and to keep the pacemaker insertion site sterile:
- You will get an IV antibiotic.
- For men: One side of your chest will be shaved..
- The procedure area will be washed.
- You will be covered with sterile drapes from your neck to your feet.
- A soft strap will be placed across your waist and arms to keep your hands from touching the sterile area.
During the Procedure
Will I be monitored?
We will use several monitors to keep track of your heart rhythm and blood pressure during the procedure.
Monitors during the procedure
Defibrillator/pacemaker/cardioverter: Patches are placed in the center of your back and on your chest. Your doctor or nurse can use the equipment connected to the patches to adjust your heart rate, if needed.
Electrocardiogram (EK): Electrode patches are placed on your chest, and inside your heart to create a picture (shown on the monitors) of the electrical impulses traveling through your heart.
Blood pressure monitor: A cuff will be placed on your arm so we can check your blood pressure during the procedure.
Oximeter monitor: A small clip will be placed on your finger to check the oxygen level of your blood during the procedure.
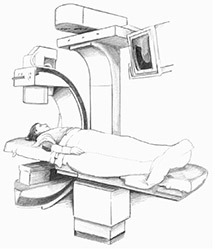
Fluoroscopy: A large X-ray machine will be positioned above you to help your doctor see the leads during the procedure.
How long does the procedure last?
The device implant procedure may last from 2 to 5 hours.
How is the device implanted?
The CRT device can be implanted using the endocardial or epicardial approach.
The endocardial (transvenous) approach is done while you are awake. A local anesthetic is injected to numb the area.
Small incisions are made in the chest where the leads and device are inserted. The leads are inserted through the incision and into a vein, then guided to the heart. Two leads are guided to the right atrium and right ventricle.
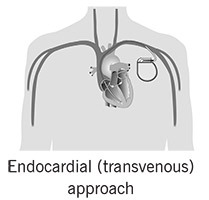
The third lead is guided through the coronary sinus to the left ventricle. The lead tips are attached to the heart muscle, and the other ends of the leads are attached to the pulse generator. The generator is placed in a pocket created under the skin in the upper chest.
What will I feel?
You will feel some stinging or burning when the doctor injects the anesthetic. Then, the area will be numb. You may feel a pulling sensation when the doctor makes the pocket for the device. Tell your doctor what you feel. You should not feel pain. If you do, let us know right away.
How long will I stay in the hospital?
Most patients leave the hospital the day after the procedure. You will stay longer if you need the epicardial surgical approach.
Not all patients are able to have the procedure using an endocardial approach due to the size, shape or location of the vein(s). The technique is also technically challenging and may not be successful.
If the endocardial approach cannot be used or is unsuccessful, the epicardial approach will be used. The epicardial approach may also be used to place the CRT if you are having surgery to treat another heart condition.
Epicardial surgical approach
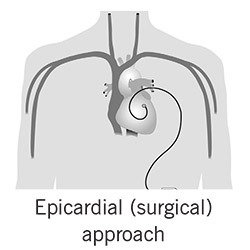
The epicardial surgical approach is done using general anesthesia. You will not feel anything during the procedure.
Two of the 3 leads are guided through the veins to the heart. These leads are guided to the right atrium and right ventricle, while the third lead is attached to the outside of the left ventricle through the ribs.
The lead tips are attached to the heart muscle, and the other ends of the leads are attached to the pulse generator. The generator is placed in a pocket created under the skin in the lower abdomen.
You will likely spend 3 to 5 days in the hospital after your procedure. Your stay may be shorter if you have minimally invasive surgery.
How are the leads tested?
After the leads are in place, they are tested to make sure they are in the right position and that they work properly. Then, the right and left ventricles are synchronized. This lead function test is called “pacing.” Small amounts of energy are delivered through the leads into the heart muscle. This energy causes the heart to contract. You will be asleep for several minutes during the lead function test.
Once the leads have been tested, your doctor will connect them to the device.
Your doctor will use a programmer on the outside of your body to adjust the device to the right settings for you.
Will I have pain after the procedure?
You may feel discomfort at the implant site during the first 48 hours after the procedure. Your doctor will tell you what medications you can take for pain relief. Please tell your doctor or nurse if your symptoms are severe or long-lasting.
After the Procedure
What should I expect during my recovery?
You will have a chest X-ray to check your lungs and the position of the device and lead(s).
We will use a telemetry monitor to keep constant track of your heart rhythm while you are in the hospital. Electrodes on your chest are connected to a small box with wires. The information from the monitor is shown on screens in the nursing unit.
You will also have a holter monitor. Like the telemetry monitor, electrodes are connected to a small box with wires. The device records your heart rhythm for 12 hours to make sure the pacemaker is working properly. The monitor will be removed before you leave the hospital, and you will go to the Device Clinic.
What happens at the Device Clinic?
You will be seen in the Device Clinic to make sure your device is adjusted to the proper settings.
You will sit in a reclining chair. Electrodes will be placed on your chest and connected to a computer. A nurse will place a small device called a programmer directly over the CRT device. The programmer is used to check the device, leads and change the device settings. You may feel your heart beat faster or slower. Although this is normal, please tell the nurse what you feel.
Your doctor will review the results and determine the right settings for you. The holter monitor results also are reviewed while you are in the Device Clinic.
You may have an echocardiogram at this time or at your next follow-up appointment.
You will get instructions about how to take care of your incision, activity guidelines and follow-up appointments.
You will also receive a temporary ID card with information about your device and procedure. Carry this card with you at all times in case you need medical care. You will get a permanent card from the pacemaker company within 3 months.
Before you leave the hospital, make sure you know which medications you need to take. You may need to make changes.
Can I drive myself home?
No. For your safety, a responsible adult must drive you home. Please have your driver at the hospital by 10:00 a.m. on the morning you are discharged.
Ask your doctor how long you need to wait before driving again.
If You Have Questions
If you have a medical emergency, call 911!
If you have symptoms that might be related to your device (dizziness, palpitations, fast or slow heart beats), you can send a remote telephone transmission (cell or land line).
Telephone transmitter line: 1.800.603.7169
For nonurgent questions: ask your doctor.