Many patients who have arrhythmias have feelings of depression and anxiety, even if they never had these feelings before. Learning you have a condition such as atrial fibrillation or ventricular tachycardia can be overwhelming. You may have a lot of questions about your diagnosis, treatment and how the condition will affect your life. Your family and caregivers may also have some of these emotions. Fortunately, your healthcare provider can recommend ways to help you cope as you make both an emotional and physical recovery from your arrhythmia intervention.
The heart-brain connection
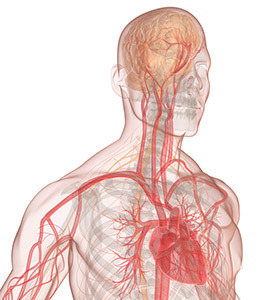
Having both clinical depression and cardiovascular disease often leads to poor outcomes. This suggests that there is a connection between the brain and the heart. The effect of heart disease on the brain is also recognized by the American Heart Association, which recommends that all cardiology patients be screened for depression. Many patients with heart disease also have anxiety. This can make cardiovascular disease worse.
Strong emotions, including high levels of anger and emotional stress, can affect your heart’s rhythm. Patients who know they have an arrhythmia are often anxious, apprehensive, worried and very sensitive to sensations in their bodies. Patients with an arrhythmia who also have a history of depression or anxiety often experience depression or anxiety after they learn they have an arrhythmia, even if they had no symptoms before the diagnosis. These symptoms can also become worse.
Because so many patients with heart disease experience depression and anxiety, it is important to let your healthcare provider know how you’re feeling throughout your treatment. He or she wants to know if you are feeling depressed or anxious and how your feelings affect your daily life. For instance, whether you enjoy life and carry out daily activities like you did before you were diagnosed with or treated for an arrhythmia. Your healthcare provider also wants to know how the people around you think you are coping.
Recognizing depression and anxiety
It is important to identify a depressive or anxiety disorder as soon as possible. Doing so helps your overall well-being. It also allows you to get early treatment, which can improve your overall quality of life. Early treatment may also improve your arrhythmia.
Screening questions for depression
- In the last couple of weeks, have you had little interest or pleasure in doing things?
- Have you been feeling down, depressed, or hopeless?
Answering yes to both of these clinical questions means it is very likely that you may be suffering from depression.
Screening questions for anxiety
- In the last couple of weeks, have you been feeling nervous, anxious or "on edge?"
- Have you had difficulty in not being able to stop or control worrying?
Answering yes to both of these clinical questions means it is very likely that you may be suffering from anxiety.
Getting help
The first step to treating depression or anxiety is to talk to a member of your cardiology healthcare team. Bring up your emotional well-being during a visit or at any time during your course of treatment. Your physician, nurse practitioner, physician assistant or nurse can review the emotional symptoms you are having and develop a treatment plan, if needed. The treatment recommendations and follow-up care you need are based on your symptoms and health history. In addition, you can also ask for a referral to a behavioral health specialist who is an expert in treating patients with arrhythmias.
Treatment options
Therapy
Short-term individual coaching therapy can help patients who are “feeling down,” have little interest in normal activities, are nervous or are unable to stop worrying. This type of therapy is led by a qualified therapist (psychologist, clinical counselor or social worker). Coaching techniques include cognitive behavioral therapy (CBT) and relaxation techniques.
Patients practice mental exercises at home to learn how to cope with their arrhythmia. These techniques involve controlling negative emotions and keeping them from becoming severe when they experience arrhythmias. Patients are also encouraged to follow basic principles of healthy living (proper foods and exercise) and to be socially connected, rather than isolated.
Medication
Sometimes, emotions related to having an arrhythmia can have a very negative effect on your quality of life. In this case, your doctor may suggest you take medication to treat your symptoms. There are medications to safely treat both depression and anxiety that can be used along with the medications you take for your heart condition.
If you are currently being treated with medication for depression or anxiety, it is important that you continue your treatment and also be treated for your arrhythmia. It is important to tell your cardiology healthcare team about any medications you are taking for depression, anxiety or any other behavioral condition.
Selective serotonin reuptake inhibitors (SSRIs) are a type of antidepressant that is very safe and effective for patients with heart disease. Sertraline, citalopram and escitalopramare are SSRIs that have been well-studied in patients with heart disease. The research shows they are safe to take along with medications for heart disease and other conditions. If you take warfarin (Coumadin®), you will need to have your blood checked regularly while taking an SSRI.
Benzodiazepines are commonly used to treat distress and anxiety. Alprazolam and lorazepam are two such medications. These are effective and safe to take with antidepressants and medications for heart disease and arrhythmia.
Support groups
Talking with patients who have a similar health history can help you cope with your arrhythmia. Support groups can be in-person or online. Ask your cardiology healthcare team for a list of resources.
For more information about emotions and arrhythmia, please see the Coping with Arrhythmias page.