What is a cardiac catheterization?
A cardiac catheterization is an invasive procedure that is used to evaluate your heart. The procedure is done in the Cardiac Catheterization Laboratory by a doctor specially trained in cardiovascular invasive procedures and a team of cardiology fellows, nurses and technicians.
The information gathered from the catheterization can be used to make a decision about the best treatment for you, such as a stent, cardiac surgery or other treatment option. A catheterization is used to find out:
- If you have coronary artery disease that affects blood flow to your heart muscle.
- If you have valve disease.
- How well your heart muscle is working and if there is fluid build-up.
How is a catheterization done?
Before the catheterization
You will get medication to make you sleepy, but you will not be asleep for the procedure. The catheter will be inserted through a small incision in your leg, arm, wrist or neck, depending on the type of evaluation you need. The area will be numbed before the incision is made.
During the catheterization

The catheter is guided through the blood vessel to the coronary arteries, heart and/or lungs. A special X-ray machine helps the doctor see the catheter.
A dye (contrast material) is sent through the catheter, and the X-ray machine captures video and pictures as the dye moves through the chambers of your heart (atria and ventricles), heart valves and major blood vessels. This part of the procedure is called a coronary angiogram (or coronary angiography). These images show any narrow or blocked areas in your coronary arteries.
Words to Know
- Arteries - Blood vessels that carry blood away from the heart.
- Atherosclerosis (“hardening of the arteries”) - The build-up of plaque inside
the arteries. - Blood vessels - The three main types of blood vessels are arteries, veins and capillaries. Blood vessels carry blood to and from parts of your body.
- Catheter - A long, thin tube that is inserted into a blood vessel.
- Coronary arteries - Arteries that carry oxygen-rich blood to the heart.
- Coronary artery disease - The leading cause of death in the United States. The coronary arteries become narrow and blocked by atherosclerosis.
- Interventional procedure - A nonsurgical procedure used for treatment (see more about this on the back of this handout).
- Plaque - A sticky substance that builds up inside the arteries, leading to coronary artery disease.
The catheterization itself takes about 30 minutes. Interventions can add time to the procedure. Please plan to stay at Cleveland Clinic the entire day.
IVUS and FFR
Your doctor may also use intravascular ultrasound (IVUS), instant wave-free ratio (IFR) or fractional flow reserve (FFR) to get more detailed images of the walls of your blood vessels. These procedures are only available in specialized hospitals and research centers.
IVUS: A tiny ultrasound probe (transducer) is placed on the tip of the catheter. As the catheter moves through the coronary arteries, high-frequency sound waves create detailed images of the inside walls of the arteries. These images show the location and amount of plaque in the arteries. Plaque is a sticky substance that builds up inside the arteries and causes coronary artery disease.
IFR/FFR: A special wire is threaded through the artery. During FFR, medication may be used to expand the artery so the blood pressure in the artery can be measured. Medication is not used to take the measurements during IFR.
Interventional treatments and surgery
An interventional treatment is often done at the same time as the catheterization. These procedures may also be scheduled after the catheterization. Common interventions are:
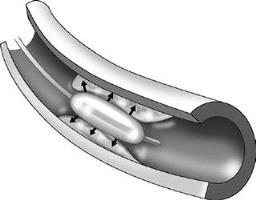
Angioplasty
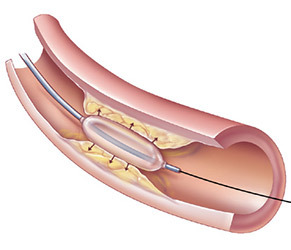
Angioplasty opens narrowed coronary arteries to improve blood flow to the heart. This is done with a special catheter that has a tiny balloon at the tip. The balloon is inflated, and the plaque build-up is pressed into the walls of the artery, which opens the artery to improve blood flow. Angioplasty is also called percutaneous transluminal coronary angioplasty (PTCA) or percutaneous coronary intervention (PCI).
Cutting balloon angioplasty
Cutting balloon angioplasty also uses a balloon-tip catheter. But, the balloon contains small blades that cut into the plaque before the balloon presses it into the artery walls.
Rotoblation
Rotoblation is also called percutaneous transluminal rotational atherectomy (PTRA). Your doctor may use rotoblation if you have heavily calcified blockages in your arteries. A special catheter with a grinding tip is guided to the blockage, and the tip spins to clear out the plaque. The particles that are ground away are microscopic. They wash away in your bloodstream and are filtered out by your liver and spleen.
Stenting
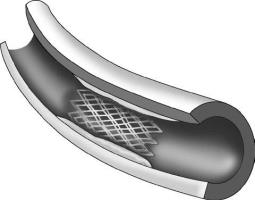
A stent is a small metal, mesh tube that acts like scaffolding to keep the artery open. Stents are usually put in place after angioplasty or rotoblation.
There are two types of stents — drug-eluting stents (DES) and bare-metal stents.
Drug-eluting stents (DES) have a thin layer of medication on them that helps keep the artery from becoming narrow again (restenosis).
Patients with DES need to take long-term antiplatelet medication to thin their blood and prevent blood clots from forming on the stent.
Bare-metal stents do not have a layer of medication. They are not used very often.
Please talk to your doctor if you:
- Currently take blood thinners.
- Plan on having any procedure or surgery within the next year that requires you to stop taking blood-thinning medication.
- Have had bleeding problems in the past.
- Have any concerns about stents.
This information will help your doctor choose the best type of stent to meet your needs.
It is very important to take all medications, including “blood thinners,” as prescribed. Do not stop taking any medication without talking your doctor.
After the procedure
You will get information about your recovery, including restrictions, problems to look for and medications you need to take after your procedure. Please review this information before you leave the hospital and let your doctor or nurse know if you have any questions or concerns.
What are the risks of catheterization and interventional procedures?
Your cardiologist will talk to you about the risks and benefits of catheterization and interventional procedures before you consent to the procedure(s). Some of the possible risks include:
- Allergic reaction to the medication or contrast material used during the procedure.
- Irregular heart rhythm.
- Infection.
- Bleeding at the catheter insertion site.
- Continued chest pain or angina.
- Mild-to-moderate skin reactions (like a sunburn) from X-ray exposure.
- Kidney failure.
- Heart attack, blood clots, stroke or death.
- Acute closure of coronary artery.
- Emergency coronary artery bypass graft (CABG) surgery.
Please make sure you understand the risks and benefits and share your questions and concerns with your doctor.
Experience is important
Catheterization and interventional procedures require special expertise. Physician credentials and experience lead to better outcomes.
Cleveland Clinic Experience: Coronary angiography was pioneered at Cleveland Clinic in 1958 by F. Mason Sones, MD, in whose honor the Cardiac Catheterization Laboratory is named.
More than 45 procedures are performed at Cleveland Clinic every day. We average about 10,000 diagnostic cardiac catheterizations and 3,000 interventional procedures every year.