What is atrial fibrillation?
Atrial fibrillation (AF or AFib) is a very fast, chaotic heart rhythm that starts in the upper chambers of your heart (atria). It can come and go (paroxysmal) or be constant (persistent).
How does AFib happen?
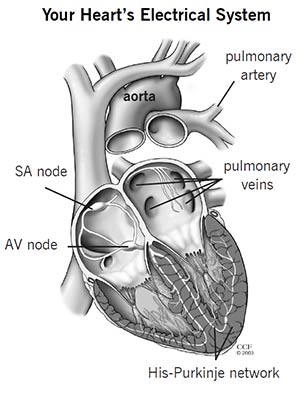
Your heartbeat is controlled by an electrical system in your heart. During a normal heartbeat, blood flows from the atria to the bottom chambers of your heart (ventricles), and then out to the rest of your body. This happens as an electrical impulse travels from the sinoatrial (SA) node, through the atria, to the atrioventricular (AV) node, through the ventricles.
If everything is working as it should, your heart beats between 60 and 100 times per minute.
When you have AFib, many electrical impulses start at the same time and spread through the atria. They all try to travel to the AV node, and it causes your heart rate to beat out of rhythm and very fast — sometimes up to 300 to 600 beats per minute.
Is AFib dangerous?
Many people with AFib live for years without any problems. But, AFib can be very dangerous.
- AFib affects blood flow out of your atria. Blood can collect in the atria and left atrial appendage (LAA) and clot, which can lead to a stroke.
- AFib can make your heart weaker and lead to heart failure.
What symptoms does AFib cause?
Not everyone with AFib has symptoms. You may:
- Feel sudden pounding, fluttering or a racing feeling in your chest (heart palpitations).
- Have chest pain, pressure or discomfort.
- Get very tired, dizzy or short of breath.
If you have symptoms of AFib, call your healthcare provider. You will have an exam and tests to check your heart rate and rhythm.
What tests will I need?
- Electrocardiogram (ECG/EKG): Small sticky patches called electrodes are attached to your chest. Wires connect the electrodes to the ECG machine. The machine measures your heart’s electrical activity and prints out a picture of it on graph paper.
- Portable monitor: You may need to wear a portable monitor to collect information about your heart rate, rhythm and your symptoms over a period of time.
What causes AFib?
Common causes of AFib are:
- High blood pressure (hypertension).
- Coronary artery disease.
- Heart valve disease.
- Heart surgery (AFib can happen after surgery).
- Chronic lung disease.
- Heart failure.
- Cardiomyopathy.
- Congenital heart disease.
- Pulmonary embolism.
- Sleep apnea - talk to your healthcare provider if you think you may have this condition.
- Obesity.
Less common causes include:
- Overactive thyroid (hyperthyroidism).
- Pericarditis.
- Viral infection.
AFib can also be related to:
- Alcohol use
- Having a lot of caffeine
- Stress
- Some drugs
- An electrolyte or metabolic imbalance
- Severe infections
- Genetic factors
- Age - your risk gets higher as you get older, especially after you turn 60.
Sometimes the cause of AFib is unknown.
Treatment for AFib
Your healthcare provider will talk to you about the best treatment plan for you.
Medicine
Medicine is a common first step in treatment for AFib. Depending on your symptoms, you may need to take medicine to:
- Control your heart rhythm
- Control your heart rate
- Prevent blood clots
Your healthcare provider will talk to you about the medicine you need and how to take each one. Please make sure share any questions or concerns you have.
Lifestyle changes
Some lifestyle habits can cause AFib or make it worse. To help control AFib:
- Do not smoke or use any form of tobacco or nicotine.
- Limit the amount of alcohol you drink. Ask your healthcare provider how much you can safely drink.
- Limit the amount of caffeine you have.
- Avoid cough and cold medications that contain stimulants. Ask your healthcare provider or pharmacist which medications are safe for you to take.
- Reach and maintain a healthy weight.
- Tell your healthcare provider if certain activities seem to trigger your AFib.
Procedures and Devices
If you still have AFib after taking medicine and making lifestyle changes, you may need a procedure or device to help your heart return to a normal rhythm. Procedures include:
- Cardioversion to shock your heart back into a normal rhythm.
- Ablation to block abnormal electrical impulses in your heart.
- Removing or blocking your left atrial appendage (LAA).
Devices include:
- A pacemaker to control your heart rate.
- A clip or other device to block blood flow between your left atrium and LAA.
What is the left atrial appendage?
Your left atrial appendage is an ear-shaped sac on the outside of your left atrium.
If you have AFib, blood can collect and form clots in your LAA. This can lead to stroke.
Your doctor may prescribe a blood thinner to reduce your risk of clots and stroke or recommend a procedure to remove or block your LAA.