What is an arrhythmia?
An arrhythmia (also called a dysrhythmia) is an irregular or abnormal heartbeat.
What are the types of arrhythmias?
- Tachycardia: A fast heart rhythm more than 100 beats per minute.
- Bradycardia: A slow heart rhythm less than 60 beats per minute.
- Supraventricular arrhythmias: Arrhythmias that start in the upper chambers of your heart (atria) or in the electrical bridge between the upper and lower chambers of the heart (ventricles).
- Ventricular arrhythmias: Arrhythmias that start in ventricles.
- Bradyarrhythmias: Slow heart rhythms that may be caused by disease in your heart’s electrical conduction system.
What causes arrhythmias?
- Coronary artery disease.
- High blood pressure.
- Heart muscle disease (cardiomyopathy).
- Heart valve disease.
- Electrolyte imbalances in the blood, such as sodium or potassium.
- Aging.
- Heart damage from a heart attack.
- The healing process after heart surgery.
- Other medical conditions.
- Stimulants (caffeine, nicotine, some medicine, etc.).
- Reactions such as shock, fear and stress.
Heart rhythms on ECG
Your heartbeat is controlled by electricity that moves through your heart. An electrocardiogram (ECG/EKG) captures information about your heartbeat and creates a graph. Each wave represents a full heartbeat.
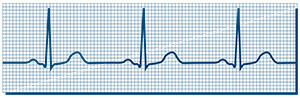
Normal Heart Rhythm/Normal Sinus Rhythm
The heart’s electrical activity is following the normal pathway. The rhythm is regular and is 50 to 100 beats per minute.
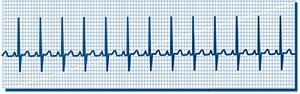
Tachycardia
Fast heart rhythm (more than 100 beats per minute).
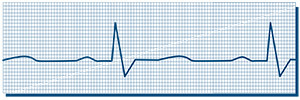
Bradycardia
Slow heart rhythm (less than 60 beats per minute).
Types of supraventricular arrhythmias
- Premature atrial contractions (PACs): Early, extra heartbeats that start in the atria.
- Paroxysmal supraventricular tachycardia (PSVT): A fast but regular heart rhythm that starts in the atria. This type of arrhythmia starts and stops suddenly.
- Accessory pathway tachycardias (such as Wolff-Parkinson-White syndrome): A fast heart rhythm caused by an extra, abnormal electrical pathway or connection between the atria and ventricles. The impulses travel through the extra pathways as well as the usual route. This lets the impulses travel very quickly inside your heart, causing an unusually fast heartbeat.
- AV nodal re-entrant tachycardia (AVNRT): A fast heart rhythm that happens when there is more than one pathway through the AV node.
- Atrial tachycardia: A rapid heart rhythm that starts in the atria.
- Atrial fibrillation (A-fib): A very common irregular heart rhythm. Many impulses start in and spread through the atria, competing for a chance to travel through the AV node. This causes a disorganized, fast and irregular rhythm. Because the impulses are traveling through the atria in a disorderly fashion, the atria can’t contract like they normally do.
- Atrial flutter: An arrhythmia caused by an electrical circuit problem in the atria. Atrial flutter is usually more organized and regular than atrial fibrillation.
Types of ventricular arrhythmias
Types of ventricular arrhythmias include:
- Premature ventricular contractions (PVCs): Early, extra heartbeats that start in your ventricles. Most of the time, PVCs don’t cause any symptoms or require treatment. This type of arrhythmia is common and can be related to stress, too much caffeine or nicotine, or exercise. They can be also be caused by heart disease or electrolyte imbalance.
- Ventricular tachycardia (V-tach): A fast heartbeat that keeps your heart from filling with enough blood, so there is less blood to pump through your body. V-tach can be serious, especially if you have heart disease. It can also cause more symptoms than other arrhythmias do.
- Ventricular fibrillation (V-fib): An erratic, disorganized firing of electrical impulses. The ventricles quiver and can’t contract like they should. This keeps your body from getting enough blood. V-fib is a medical emergency that requires treatment right away!
- Long QT: The QT interval is the area on the ECG that represents the time it takes for your heart muscle to contract and recover. If your QT interval is longer than normal, you have an increased risk of a life-threatening form of ventricular tachycardia called torsade de pointes.
Types of bradyarrhythmias
Types of bradyarrhythmias include:
- Sinus node dysfunction: Slow heart rhythms due to an abnormal SA node.
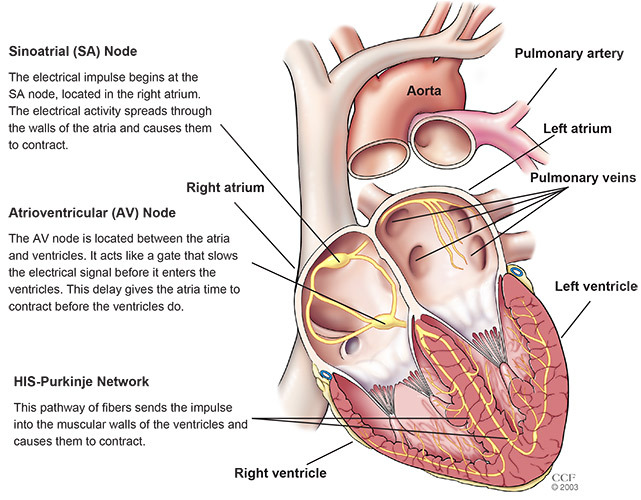
- Heart block: A delay or complete block of the electrical impulse as it travels from the sinus node to the ventricles. The delay or block can happen in the AV node or the HIS-Purkinje network.
How does an arrhythmia make me feel?
An arrhythmia may not cause any symptoms, but symptoms include:
- Palpitations: These can feel like your heart is racing, pounding, flip-flopping, fluttering or skipping beats.
- Feeling dizzy or light-headed.
- Feeling short of breath.
- Chest discomfort.
- Feeling weak or very tired (fatigue).
If you have symptoms of an arrhythmia, it is best to see a cardiologist or electrophysiologist — a cardiologist who specializes in diagnosing and treating patients with heart rhythm disorders.
The heart’s electrical system
During each heartbeat, your heart’s upper chambers (atria) and lower chambers (ventricles) work together, taking turns squeezing (contracting) and relaxing to pump blood through your heart. This pattern is controlled by your heart’s electrical system.
How do I know if I have an arrhythmia?
A cardiologist or electrophysiologist can find out if you have an arrhythmia by checking your pulse, listening to your heart or with tests.
Some tests that can find and give more information about an arrhythmia are:
- Electrocardiogram (ECG/EKG): A picture of the electrical activity in your heart. Small sticky patches (electrodes) are attached to your skin. Wires carry the information from the electrodes to the ECG machine. The machine prints a graph of the information.
- Ambulatory monitors: These portable devices record your heart rhythm and rate for 24 hours or longer.
- Stress test: Exercise or medication is used to make your heart beat faster and show how it reacts. This test is used to find out more about arrhythmias that start or get worse when you exercise. It can also detect heart disease that is causing your arrhythmia.
- Echocardiogram (echo): An ultrasound that shows the inside of your heart. This test is used to look for heart muscle or valve disease that may be causing your arrhythmia. You may have an echo while you are resting or exercising.
- Cardiac catheterization (cath): This invasive test uses a long, thin tube (catheter) to check the inside of your blood vessels and heart. The catheter is inserted through a small incision in your groin, arm or wrist and guided to your heart using X-ray. Contrast dye is used to check blood flow and help identify heart disease.
- Electrophysiology study (EPS): A special heart catheterization that evaluates your heart’s electrical system. Catheters are inserted into your heart to record the electrical activity. The EPS is used to find the cause of the abnormal rhythm and determine the best treatment for you. During the test, the arrhythmia can be safely reproduced and terminated.
- Tilt table test: You will lie on a table that is moved to different angles. As this happens, your blood pressure and heart rate are measured minute-by-minute to see how your body responds.
If you have an arrhythmia, it is a good idea for your family members to know the symptoms of an arrhythmia, what to do, and how to do CPR.
How do I take my pulse?
You can feel your pulse on your wrist or neck. Place the tips of your index and middle fingers on the inner wrist of your other arm, just below the base of your thumb.
Or, place the tips of your index and middle fingers on your lower neck, on either side of your windpipe. Press lightly with your fingers until you feel the blood pulsing. You may need to move your fingers up or down a little to feel your pulse.
Count the number of beats in 10 seconds and multiply that number by 6 to find out how many times your heart beats per minute. A normal heart rate, at rest, is 50 to 100 beats per minute.
What treatment do I need for my arrhythmia?
Treatment for your arrhythmia depends on the type you have an how severe it is. You may not need any treatment. But if you do, you may need to make lifestyle changes, take medicine, have a procedure, get a device or have surgery.
No matter which type of treatment you need, it is very important to keep all follow-up visits with your healthcare team and follow your plan of care. Please let your doctor know if you have any questions or concerns.
Lifestyle changes
Arrhythmias can be caused by things other than heart disease. Your doctor will talk to you about making changes, if needed, such as:
- Not smoking.
- Limiting the amount of alcohol you drink.
- Limiting or avoiding caffeine and other stimulants.
Medications
You may need to take medicine to:
- Get your heart back into a normal rhythm.
- Prevent an arrhythmia.
- Control your heart rate.
- Prevent blood clots.
Procedures
Your doctor may talk to you about a procedure if medicine does not stop your arrhythmia. These are:
- Cardioversion: This procedure uses an electric shock to get your heart back into a normal rhythm.
- Catheter ablation: A catheter is used to deliver energy to kill tiny areas of your heart muscle that cause your arrhythmia. This disconnects the pathway of the abnormal rhythm. An ablation can also disconnect the electrical pathway between the atria and ventricles. The type of ablation used depends on the type of arrhtythmia you have. Ablation is most often used to treat patients with PSVT, A-fib, atrial flutter, AVNRT and V-tach. Ablation is sometimes combined with other procedures.
Devices
You may need to have an implanted device to keep your heart beating normally. These include:
- Permanent pacemaker: A device that sends small electrical impulses to your heart muscle to keep your heart rate normal. Pacemakers are used most often to keep your heart from beating too slowly.
- Implantable cardioverter-defibrillator (ICD): An electronic device that constantly monitors your heart rhythm. When it detects a very fast, abnormal heart rhythm, it sends energy to the heart muscle. This causes the heart to beat in a normal rhythm again. There are different types of ICDs. If you need this device, your doctor will talk to you about the best option for you.
Surgery
If your arrhythmia continues after you try other treatment options, you may need surgery to correct your heartbeat. The Maze and modified Maze procedures are two procedures used to treat patients with atrial fibrillation. You may also need surgery if you have other types of heart disease, such as coronary artery or valve disease.