What is atrial fibrillation ablation?
Atrial fibrillation ablation is a treatment for some patients with atrial fibrillation (AFib). The procedure is also called pulmonary vein isolation (PVI).
Who can have atrial fibrillation ablation?
An ablation may be a good treatment option for you if you have AFib symptoms even after taking medicine to control your heart rate and rhythm. An ablation can also be a good treatment option if you have symptoms and:
- Can’t take medicine for AFib because you get side effects from it.
- Don’t want to take medicine for AFib.
- Are concerned about taking AFib medicine for a long time.
- Have heart failure or your heart muscle is weak.
If you are interested in having an ablation at Cleveland Clinic, you will need a detailed evaluation that includes tests to get more information about your AFib and heart. If your cardiologist is outside of Cleveland Clinic, call 216.444.6697 or 800.223.2273, ext. 46697 to schedule an evaluation. You can also schedule a virtual second opinion. Visit my.clevelandclinic.org/online-services/virtual-second-opinions for details.
How does an atrial fibrillation ablation work?
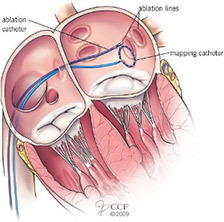
The ablation uses either heat (radiofrequency) or cold (cryoablation) energy to target the part of your heart where the AFib starts. This is usually the area where your pulmonary veins connect to the top left chamber of your heart (left atrium). This is why the procedure is also called PVI. But, other areas may also be targeted.
The energy kills the tissue, which causes protective scars to form. It takes about 2 to 3 months for the scars to fully develop. The scars block the electrical impulses that cause AFib from firing in your pulmonary veins. This disconnects them from your heart and prevents AFib. Your heart’s electrical pathway is then normal, so your sinus node can direct your heart rhythm, like it should, and your heart rate and rhythm go back to normal.
What happens during an atrial fibrillation ablation?
Before the ablation
- The procedure is done in the Electrophysiology (EP) Lab.
- A nurse will help you get ready.
- We will wash your groin and chest with an antiseptic solution.
- We will shave the incision area.
- We will cover you from your neck to your feet with sterile paper sheets (drapes).
- You will meet your healthcare team members during a “huddle” before the ablation. Please let us know if you have any questions or concerns.
- Most patients get general anesthesia to “go to sleep” during the ablation. Your doctor will talk to you before the day of the procedure about the best type of anesthesia for you.
- You will get an IV to give you fluids and medication during the procedure.
Equipment and monitors used during the ablation
Many of the monitors use sticky pads (electrodes) that are placed on your body and attached to the equipment with wires.
- Ablation machine: The source of the energy used during ablation.
- Blood pressure monitor: Used to check your blood pressure during the procedure.
- Defibrilator/pacemaker/cardioverter: Used to adjust your heart rate as needed during the procedure.
- Electrocardiogram (ECG/EKG): Used to keep track of your heart rate and rhythm during the procedure.
- Fluoroscopy: An X-ray machine above you helps your doctor guide the instruments during the procedure.
- Mapping system: Advanced technology to help your doctor find the exact area(s) causing your Afib.
- Oximeter: A small clip on your finger used to keep track of the oxygen level in your blood.
- Temperature probe: A monitor that goes into your throat (esophagus/”food pipe”) to make sure your esophagus doesn’t get too hot or cold because of the energy used during the ablation.
During the ablation
- The ablation is done through long thin tubes called catheters. These include:
- A catheter guided to the top right chamber of your heart (right atrium) to find the abnormal impulses coming from your pulmonary veins.
- Catheters to deliver energy. If your doctor is using cryoablation, a tiny balloon at the tip of the catheter will deliver the cold energy.
- An ultrasound catheter so your doctor can see inside your heart and put the other catheters in the right place.
- Your doctor will make a small incision in your groin and insert the catheters into your femoral artery, and they are guided to your heart.
- When the catheters are in place, the energy is delivered to the problem areas and then removed.
- The ablation can take 3 to 6 hours. This includes the time it takes to get you ready for the procedure, the ablation itself and time to control bleeding from the insertion sites after the catheters are removed.
What happens after an atrial fibrillation ablation?
You will lie on your back for 2 to 6 hours after the procedure. You will either go home the same day or spend the night in the hospital. Please make sure you arrange for a responsible adult to drive you home.
We will give you discharge instructions that detail your restrictions, how to care for yourself, signs of a problem and who to call if you have questions or concerns.
What type of follow-up care do I need?
It is very important to keep all follow-up visits after your ablation. We will let you know ahead of time if you need to have tests or follow special instructions before your appointments.
Your first visit will be with your doctor 3 to 4 months after the procedure. We will schedule this appointment for you. If you do not get appointment information within 3 weeks after your ablation, please call us at 216.444.6697 or 800.223.2273, ext. 46697.
You will have another appointment with a nurse practitioner (NP) or physician assistant (PA) one year after your ablation.
What are the risks of atrial fibrillation ablation?
Atrial fibrillation ablation is generally a very safe procedure. But, there are risks of problems with all procedures. Your doctor will talk to you before the procedure about your specific risks and benefits of an ablation. Please make sure you ask questions and understand your risks.
At Cleveland Clinic, the risk of a severe or life-threatening complication is between 1% and 3%. the risk of dying from a complication is less than 1 in 5,000. There is a 0.5% risk of stroke, narrowing of your pulmonary veins or a hole/tear in your heart. Some other possible risks include damage to your esophagus (less than 0.1%) and damage to the nerve that helps control breathing (phrenic nerve).
We use advanced techniques, safety precautions and monitoring to do everything possible to reduce your risk of problems. In the event of a problem, we are ready to immediately do everything possible to correct the situation.
How well does atrial fibrillation ablation work?
The success of your ablation depends on the type of AFib you have, other heart problems you have and other factors. Your doctor will talk to you before the procedure about what to expect.
It is common to have abnormal heartbeats until the scars are fully formed. They usually go away within a week after the ablation, but can last up to 8 weeks. These arrhythmias do not mean the ablation did not work.
It is rare, but your AFib may get worse for a few weeks after the ablation. If this happens, your doctor will talk to you about medications or a procedure to control your heart rate and rhythm.
An ablation is most successful for patients who have AFib that comes and goes (paroxysmal) and stops within 1 to 3 days. In these cases, a single ablation is successful for 75% to 80% of patients.
The success rate for a single ablation is about 60% to 70% if you have had constant AFib for a long time or have a lot of scarring on your heart caused by other heart problems.
In general, the risk of needing another ablation to cure AFib is about 20% to 30%.
Cleveland Clinic doctors are very experienced in the treatment of patients with AFib, and outcomes for patients are excellent. For details, visit: ccf.org/outcomes.