Dislocations happen when something pushes the bones in your shoulder joint out of their usual place. Falls, sports injuries and car accidents are the most common causes. Never try to force your shoulder back into place. Keep your arm still and close to your side and go to the emergency room right away if you think your shoulder is dislocated.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
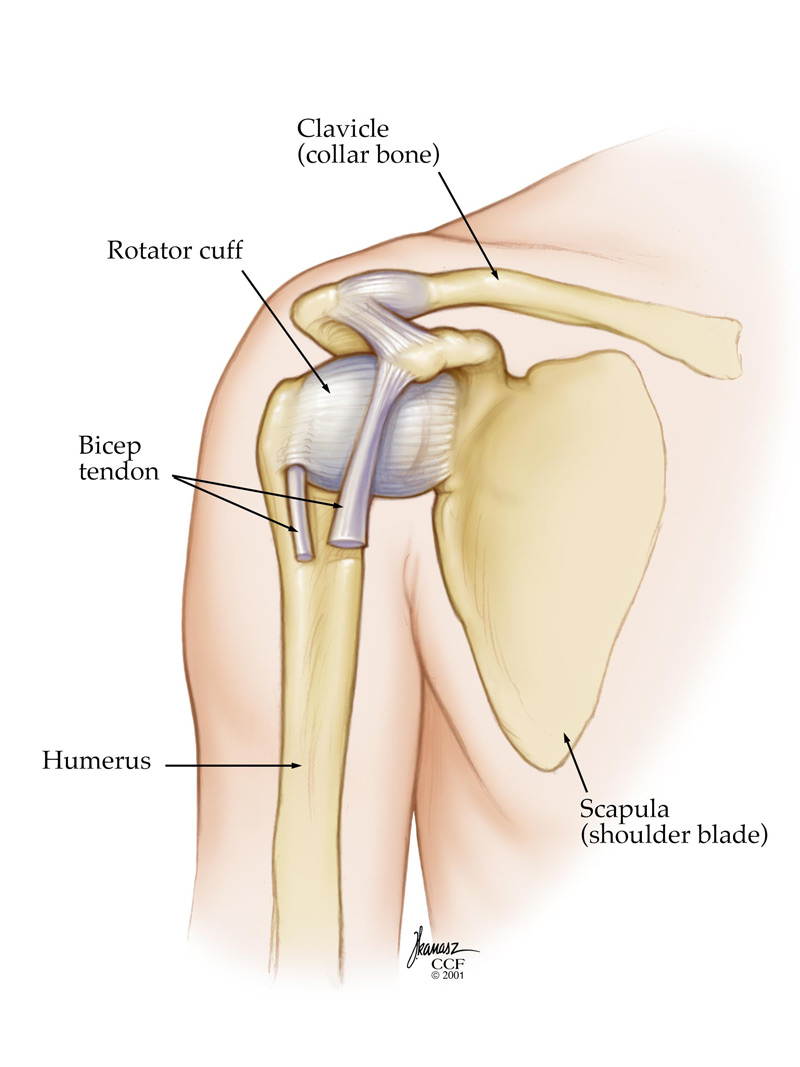
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17746-dislocated-shoulder)
Shoulder dislocations happen when the bones in your shoulder joint are pushed or knocked out of their usual places.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A joint is any place in your body where two bones meet. They’re part of your skeletal system. Your shoulder joint is where the round ball at the top of your upper arm bone (humerus) fits into the socket (glenoid) of your shoulder blade (scapula).
A shoulder dislocation is an injury that happens when the ball and socket connection between your bones is separated. It can also damage the tissue around your shoulder joint, including your:
Go to the emergency room if you experience a dislocation or can’t move your shoulder. Never try to force your shoulder back into place on your own.
Healthcare providers classify dislocations depending on how far the bones in your joints were moved:
Shoulders are the most commonly dislocated joint. But they’re still a relatively rare injury — only around 10 per 100,000 people in the U.S. dislocate a shoulder each year.
Advertisement
The most common symptoms of a dislocated shoulder include:
Any force that’s strong enough to push your shoulder joint out of place can cause a dislocation. The most common causes include:
Anyone can experience a shoulder dislocation, but some people have a higher risk than others, including:
Men are more than twice as likely to dislocate a shoulder as women.
The most common complications of shoulder dislocation are damage to the bones and tissues around your shoulder, including:
Some people who dislocate a shoulder develop a Hill-Sachs lesion. A Hill-Sachs lesion is like a dent in the ball of your upper humerus. If you dislocate your shoulder and your humerus is pressed against the lip of its socket in your scapula, the ball at the top of it can be damaged.
A healthcare provider will diagnose a dislocated shoulder with a physical exam. They’ll look at your shoulder and the rest of your arm. Tell your provider about any symptoms you’re experiencing and what you were doing right before you injured your shoulder.
Your provider might need some of the following imaging tests to diagnose damage inside your body after a dislocation:
Go to the emergency room right away if you think your shoulder might be dislocated. The most important treatment for a dislocated shoulder is getting your arm back into its socket. This is called a closed reduction or manipulation. During this nonsurgical procedure, your provider will physically push and pull your body on the outside to set (align) your shoulder. They might give you a local anesthetic to numb the area around your shoulder or sedatives to relax your whole body.
Don’t try to push your joint back in place by yourself. Don’t let anyone who’s not a trained, professional healthcare provider move or touch your injured shoulder, either. Try to hold your shoulder as still as possible and don’t force yourself to use it.
If you try to force a dislocated shoulder back in place on your own, you can make your injury worse and damage the tissue around it.
Advertisement
After your provider puts your joint back in place, you might need other treatments, including:
Advertisement
Most people don’t need surgery after dislocating their shoulders. You may need surgery if:
It usually takes a few months to recover after dislocating your shoulder. You’ll need to keep your shoulder immobilized for a few weeks and months of physical therapy after your joint has healed.
Ask your provider how long you need to wait before you resume physical activities. If you return to playing sports or working out before your shoulder has fully healed, you have an increased risk of reinjuring it — including dislocating it again.
Most people make a full recovery after dislocating their shoulder. Even if you need surgery, you should be able to return to most or all your activities and sports after your shoulder has healed.
You’re much more likely to re-injure a shoulder you’ve dislocated before. Some studies have found that more than 90% of athletes younger than 25 who dislocate a shoulder during a contact sport re-injure the same shoulder in the future.
Advertisement
Talk to your provider or surgeon before resuming any physical activities — especially contact sports. They’ll help you understand what to expect and how you can prevent future dislocations.
You might need to miss work or school while your shoulder is immobilized if you can’t do your job or schoolwork without moving your injured shoulder. Your provider will tell you which motions or positions to avoid while you’re recovering. Ask your provider when you can return to sports, doing chores or lifting heavy objects.
You can’t always prevent a dislocated shoulder. It usually happens because of unexpected accidents and trauma.
During sports or other physical activities:
Follow these general safety tips to reduce your risk of an injury:
Go to the emergency room if you’ve experienced trauma.
If you think your shoulder is dislocated:
A dislocated shoulder won’t heal on its own, and it won’t heal properly unless a healthcare provider diagnoses and treats it.
Go to the emergency room if you have any symptoms of a dislocation after a fall, sports injury or accident.
A dislocated shoulder happens when something forces the ball-shaped head of your upper arm bone out of the socket in your shoulder blade. Falls, sports accidents and other trauma usually cause dislocated shoulders. Shoulders are the most commonly dislocated joint.
Never try to pop your shoulder back in place on your own. Don’t let anyone other than a healthcare provider touch or move it. Go to the emergency room right away if you think your shoulder is dislocated or you can’t move or use your arm.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
