If you need shoulder replacement surgery (shoulder arthroplasty), your surgeon will replace some or all of your natural shoulder joint with a prosthetic. Recovery can be hard work, but most people notice dramatically reduced pain, stiffness and other symptoms once they’ve healed and adjusted to their new joints.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
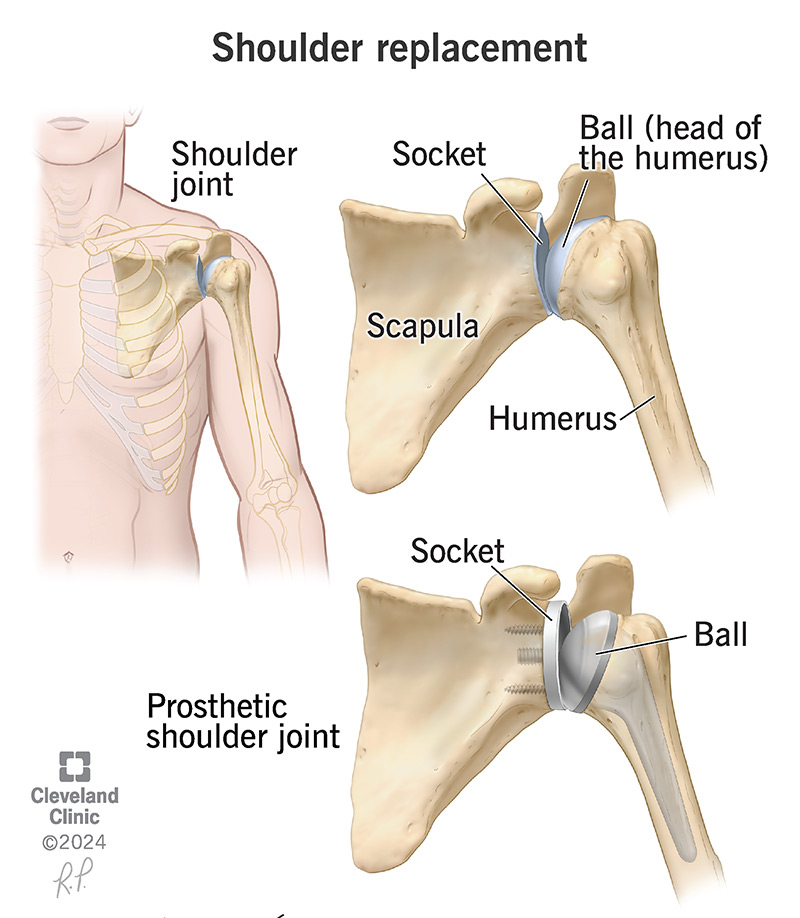
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/shoulder-replacement-surgery)
Shoulder replacement surgery is a joint replacement (arthroplasty) for your shoulder. Healthcare providers sometimes call it a total shoulder arthroplasty.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A surgeon will replace the bones and connective tissue in your natural shoulder joint with an artificial joint (a prosthesis). Prosthetic shoulders are made of metal and plastic.
Your shoulder is where your upper arm bone (humerus) connects to your shoulder blade (scapula). It’s a ball and socket joint. The ball-shaped top (head) of your humerus fits into the cup-shaped socket in your scapula (glenoid).
Most people who need shoulder replacement surgery have a total arthroplasty. Your surgeon will replace the ball at the end of your humerus and the socket in your scapula it fits into.
Your surgeon may suggest a partial shoulder replacement if only one part of your shoulder is damaged enough to need surgery. They’ll most commonly replace just the ball, if your socket isn’t damaged. This is called a hemiarthroplasty.
Partial replacements are less common. That’s because most people who have arthritis or another issue that’s severe enough to need a shoulder replacement experience damage to the whole shoulder.
A healthcare provider might suggest shoulder replacement if nonsurgical treatments haven’t helped manage severe symptoms like:
Advertisement
Most people who need a shoulder replacement have shoulder arthritis, usually osteoarthritis or rheumatoid arthritis.
Your provider may also recommend shoulder replacement surgery if you have a severe rotator cuff tear or a health condition like avascular necrosis that affects your ability to use your shoulder.
Your healthcare provider or surgeon will help you get ready for surgery. You’ll need a few tests, including:
You may have to stop taking some medications or supplements before your surgery. Tell your provider or surgeon which prescription medications you take and over-the-counter supplements you use.
Most people need to avoid eating and drinking (fast) for eight hours before their surgery. Your surgeon will tell you when you should fast the day before your surgery. They’ll also let you know which medications are safe to take with a sip of water before your surgery.
Before your surgery, an anesthesiologist will give you anesthesia to numb your body and make sure you don’t feel any pain. They may give you general anesthesia to put you to sleep, a regional anesthesia that numbs your shoulder and the area around it, or a combination of the two.
During a shoulder replacement your surgeon will:
Shoulder replacement surgery usually takes around two hours. Your surgery may take more or less time depending on how damaged your natural joint is.
Shoulder replacement surgery can drastically reduce the pain and other symptoms you feel in your shoulder. Most people can use their shoulders better or more effectively than they could before surgery (they have increased mobility).
Shoulder replacement surgery is safe and effective. Rare complications can include:
Your surgery care team will move you to a recovery room after your surgery. They’ll keep an eye on your vital signs and pain level while you recover from the anesthesia.
Some shoulder replacements are outpatient procedures (you can go home the same day). Your surgery may be inpatient, which means you’ll need to stay in the hospital at least overnight. Your care team will tell you when it’s safe for you to go home.
Advertisement
It can take a few months to recover completely after shoulder replacement. Your surgery care team will put your arm in a sling after surgery. You’ll need to wear the sling for at least a few weeks.
Your surgeon will give you exercises and shoulder movements to start regaining strength and mobility in your shoulder. Do these exercises as often as your surgeon suggests. It’s important to help your shoulder stay mobile and flexible right after surgery and as it heals.
You’ll start physical therapy a few weeks later. A physical therapist will give you exercises and stretches to help you regain your range of motion (how far you can move your shoulder) and strengthen your shoulder muscles.
Having any type of surgery hurts. You’ll feel pain in your shoulder after surgery, especially in the first few weeks. Your shoulder will hurt from the surgery itself and as your body begins to heal.
Your surgeon will suggest a combination of prescription pain medication, over-the-counter NSAIDs (if it’s safe for you to take them) and acetaminophen to relieve your pain. Your surgeon will tell you how much of each kind of medication you can take each day or in a certain amount of time.
You may need to avoid intense activities like lifting heavy objects, playing sports or working out for a few months. Most people can resume light daily activities with their shoulders (like getting dressed and doing simple chores) after two or three weeks. You can gradually increase your activity level once your surgeon says it’s safe. Check with your surgeon before resuming any physical activity that uses your shoulder.
Advertisement
A shoulder replacement usually lasts many years. Most people who have a shoulder replacement live with the prosthetic for at least 15 years. Many have it for the rest of their lives.
Some people with a shoulder replacement can only lift a certain amount of weight. You’ll have a lifting restriction while you recover. You might need to limit how much you lift with your prosthetic shoulder permanently.
Your surgeon will tell you what to expect, and what’s safe to do with your shoulder.
Call your healthcare provider or surgeon if you experience any of the following symptoms after surgery:
Shoulder replacement surgery can sound like a daunting and difficult process, but it’s worth it. Recovery and physical therapy are a lot, but don’t forget to give yourself credit for building up your strength and doing what’s necessary to get your shoulder back up to speed. It’s hard work, and you deserve to celebrate your successes as you go.
Advertisement
It’s completely normal and healthy to be nervous before surgery. Talk to your healthcare provider and surgeon. They’ll help you understand everything that will happen before, during and after the procedure.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Eliminate shoulder pain with shoulder replacement surgery at Cleveland Clinic. Our experienced providers personalize your treatment so you can move better.
