Multiple myeloma happens when healthy plasma cells become abnormal cells that multiply and produce abnormal proteins. This can cause medical issues that can affect your bones, kidneys and blood cells. Healthcare providers can’t cure multiple myeloma, but they can treat related conditions and symptoms and slow its progress.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
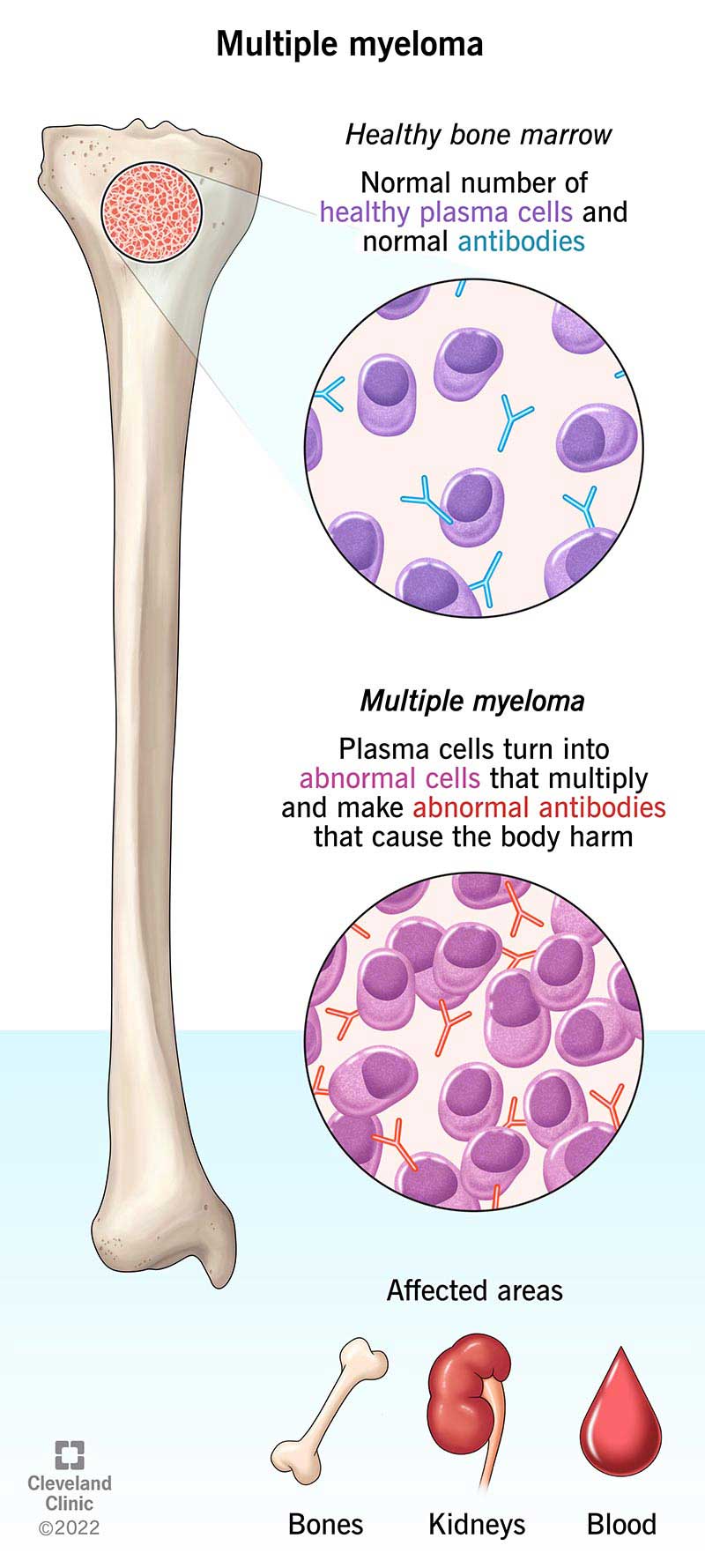
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/6178-multiple-myeloma)
Multiple myeloma is a rare blood cancer that affects your plasma cells. Plasma cells are a type of white blood cell. They make antibodies to fight infection. But with multiple myeloma, plasma cells develop errors and build up in your bone marrow. Bone marrow is the tissue inside bones that makes blood cells. The abnormal plasma cells make abnormal proteins called M proteins.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The cancerous plasma cells can crowd out your normal bone marrow cells. This can prevent your bone marrow from producing healthy red blood cells. This leads to a condition called anemia. The abnormal plasma cells can also damage your bones and kidneys.
Healthcare providers can’t cure multiple myeloma. But they can treat symptoms and related conditions that it can cause. Often, they can slow its progress, so you can live longer.
Bone pain (usually in your back, head, chest, pelvis or upper leg) is often the first symptom people notice. Other symptoms include:
Medical experts aren’t sure what causes multiple myeloma. But they do know that it happens when there’s a change (gene mutation) in your plasma cells. The mutations cause plasma cells to divide uncontrollably. These aren’t mutations you’re born with. Instead, they happen over your lifetime.
Experts are researching links between specific types of mutations and multiple myeloma. The type of mutation helps providers know how aggressive the disease is. It provides clues about how it will respond to treatment.
Advertisement
Risk factors include:
Multiple myeloma can lead to other medical issues, like:
Some complications require emergency medical care, including:
Your healthcare provider will work with you to manage or prevent these complications.
Several tests help doctors confirm a multiple myeloma diagnosis. Tests include:
Sometimes, people with multiple myeloma don’t have symptoms. Your provider may not suspect anything until blood tests show signs of conditions that may become multiple myeloma.
For example, a biopsy may show abnormal plasma cells, which could mean you have either MGUS or smoldering multiple myeloma. These are early, precancerous forms of multiple myeloma.
Advertisement
Most people with these conditions don’t develop multiple myeloma. Still, your healthcare provider will monitor you closely in case they progress.
Cancer staging lays the foundation for treatment. Healthcare providers use the Revised International Staging System (R-ISS) to stage multiple myeloma. It’s based mostly on how many cancer-related enzymes or M proteins are in your blood. Healthcare providers also consider if you have gene abnormalities.
The scale goes from I (growing slowly) to III (growing fast).
Treatment may involve several cancer therapies, with or without a stem cell transplant. A stem cell transplant may slow cancer spread drastically. But not everyone is a candidate.
Treatments include:
Advertisement
Other treatments you may need include:
Multiple myeloma treatment often involves taking a combination of cancer medications. You may take different types of high-dose chemotherapy drugs. A common combination treatment is called Daratumumab-VRd. It involves taking:
Both multiple myeloma and treatments to fight it can cause unpleasant symptoms. Some are manageable. For others, you should see your healthcare provider. Ask your provider what symptoms or side effects to expect. Make sure you know when to contact them for an appointment and when to seek emergency care.
There’s no cure for multiple myeloma. But your healthcare provider can help you manage it with treatment. Everyone’s prognosis is different. The overall five-year survival rate is 62%. This means 62 out of 100 people are alive five years after their diagnosis. But the survival rate is higher (80%) when it’s diagnosed in the early stages.
Some people live 10 years or more with multiple myeloma. Much depends on how advanced the cancer is and whether it’s considered high risk.
Advertisement
Your provider will consider these factors as they design your treatment.
If you’re living with this condition, it’s important to take things one step at a time. It can be challenging to predict how this condition will affect your body. You can’t always know how you’ll respond to treatment. This is why your healthcare provider will monitor you closely.
Follow their treatment plan. And in the meantime, take care of your body and mind. Getting enough rest and the right nutrition still matters. So does being active — at safe levels. Reach out to a therapist and support groups for emotional support as you work through this diagnosis.
Multiple myeloma treatments are helping people live longer than ever, with improved quality of life. Still, living with cancer isn’t easy. Treatment and tests will always be part of your life. But know that many others are in the same position. And they’re dealing with this condition in ways that allow them to live fully each day. Reach out to others living with cancer for support. Ask your healthcare provider for resources as you learn what living with multiple myeloma means for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a multiple myeloma diagnosis, you want experts by your side. At Cleveland Clinic, our experienced providers can custom a treatment plan for you.
