Headaches are a very common condition that most people will experience many times during their lives. The main symptom of a headache is pain in your head or face. There are several types of headaches, and tension headaches are the most common. While most headaches aren’t dangerous, certain types can be a sign of a serious underlying condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
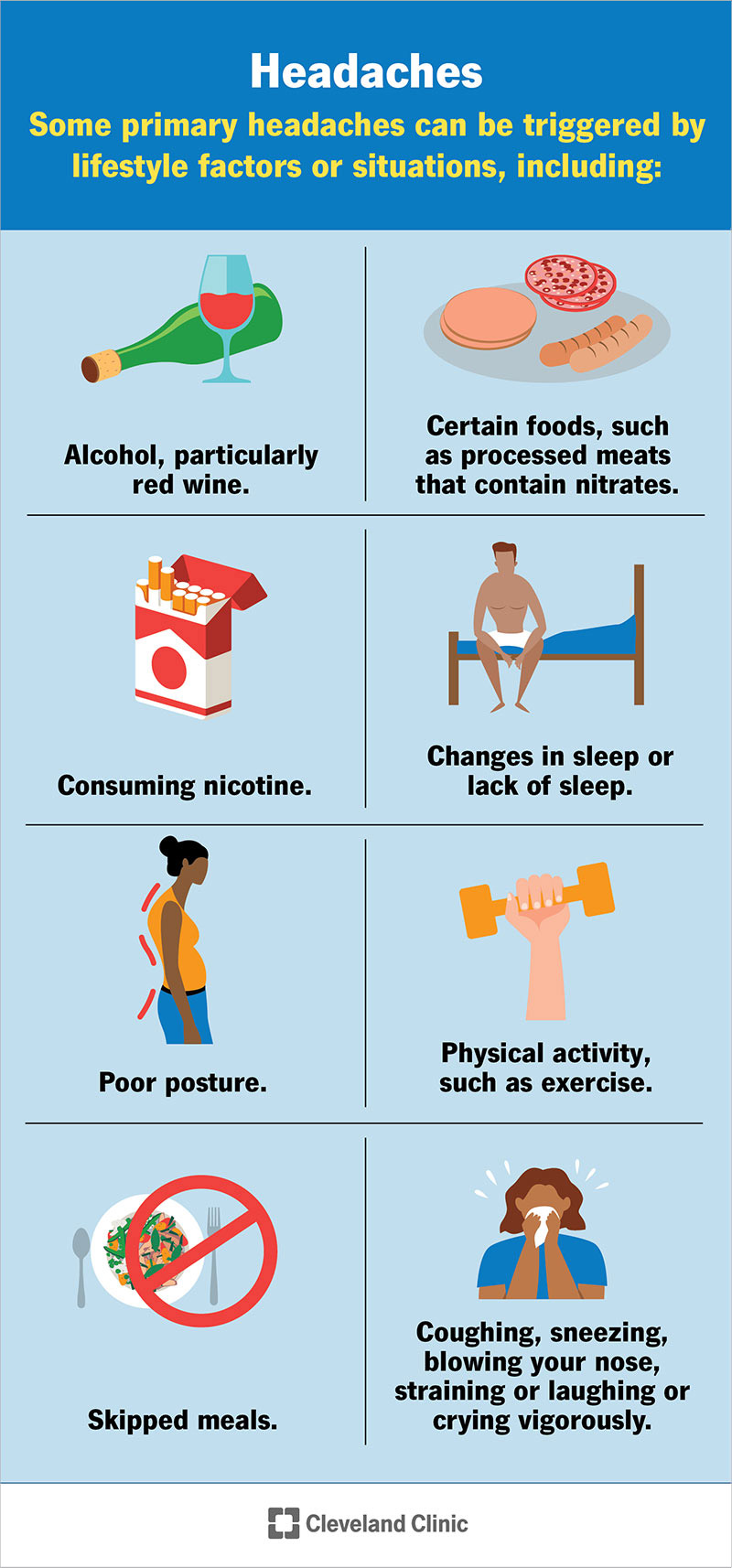
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9639-headache)
A headache is a pain in your head or face that’s often described as a pressure that’s throbbing, constant, sharp or dull. Headaches can differ greatly in regard to pain type, severity, location and frequency.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Headaches are a very common condition that most people will experience many times during their lives. They’re the most common form of pain and are a major reason cited for days missed at work or school, as well as visits to healthcare providers.
While most headaches aren’t dangerous, certain types can be a sign of a more serious condition.
There are more than 150 types of headaches. They fall into two main categories: primary and secondary headaches.
Dysfunction or over-activity of pain-sensitive features in your head cause primary headaches. They’re not a symptom of or caused by an underlying medical condition. Some people may have genes that make them more likely to develop primary headaches.
Types of primary headaches include:
Some primary headaches can be triggered by lifestyle factors or situations, including:
Advertisement
Primary headaches typically aren’t dangerous, but they can be very painful and disrupt your day-to-day life.
An underlying medical condition causes secondary headaches. They’re considered a symptom or sign of a condition.
Types of secondary headaches that aren’t necessarily dangerous and resolve once the underlying condition is treated include:
Types of secondary headaches that can be a sign of a serious or potentially life-threatening condition include:
Spinal headaches: Spinal headaches are intense headaches that occur when spinal fluid leaks out of the membrane covering your spinal cord, usually after a spinal tap. Most spinal headaches can be treated at home, but prolonged, untreated spinal headaches can cause life-threatening complications, including subdural hematoma and seizures.
Thunderclap headaches: A thunderclap headache is an extremely painful headache that comes on suddenly, like a clap of thunder. This type of headache reaches its most intense pain within one minute and lasts at least five minutes. While thunderclap headaches can sometimes be harmless, it’s important to seek immediate medical attention. They can be a sign of:
A migraine is a type of primary headache disorder.
A migraine is a common neurological condition that causes a variety of symptoms, most notably a throbbing headache on one side of your head. Migraines often get worse with physical activity, lights, sounds or smells. They usually last at least four hours or even days.
Anyone can have a headache, including children, adolescents and adults. About 96% of people experience a headache at least once in their life.
About 40% of people across the world have tension-type headaches and about 10% have migraine headaches.
Headache pain results from signals interacting among your brain, blood vessels and surrounding nerves. During a headache, multiple mechanisms activate specific nerves that affect muscles and blood vessels. These nerves send pain signals to your brain, causing a headache.
Headaches tend to run in families, especially migraines. Children who have migraines usually have at least one biological parent who also experiences them. In fact, kids whose parents have migraines are up to four times more likely to develop them.
Headaches can also be triggered by environmental factors shared in a family’s household, such as:
Advertisement
If you or your child has any of these headache symptoms, get medical care right away:
Also seek medical care right away if your headache is associated with neurological symptoms, such as:
If you have headaches often or if they’re very severe, reach out to your healthcare provider.
It’s important to diagnose headaches correctly so your provider can prescribe specific therapy to help you feel better. Your provider will complete a physical examination, discuss your medical history and talk to you about your headache symptoms. This conversation is part of a headache evaluation.
During the headache evaluation, your provider will ask you about your headache history, including:
Advertisement
Your headache can be more accurately diagnosed by knowing:
After completing the medical history part of the evaluation, your provider may perform physical and neurological examinations. They’ll look for signs and symptoms of an illness or condition that may be causing the headache, including:
Neurological tests focus on ruling out diseases that might also cause headaches. A disorder of your central nervous system might be suspected in the development of serious headaches.
Advertisement
After evaluating the results of your headache history, physical examination and neurological examination, your physician should be able to determine what type of headache you have, whether or not a serious problem is present and whether additional tests are needed.
If they’re unsure of the cause, they may refer you to a headache specialist.
Although scans and other imagining tests can be important when ruling out other diseases, they don’t help in diagnosing migraines, cluster or tension-type headaches.
But if your healthcare provider thinks that your headaches are being caused by another medical condition, there are several imaging tests they may order.
A CT scan or MRI can help determine if your headaches are connected to an issue with your central nervous system. Both of these tests produce cross-sectional images of your brain that can show any abnormal areas or problems.
Treatment for headaches depends on the type.
One of the most crucial aspects of treating primary headaches is figuring out your triggers. Learning what those are — typically by keeping a headache log — can reduce the number of headaches you have.
Once you know your triggers, your healthcare provider can tailor treatment to you. For example, you may get headaches when you’re tense or worried. Counseling and stress management techniques can help you handle this trigger better. By lowering your stress level, you can avoid stress-induced headaches.
Not every headache requires medication. A range of treatments is available. Depending on your headache type, frequency and cause, treatment options include:
Stress management teaches you ways to cope with stressful situations. Relaxation techniques help manage stress. You use deep breathing, muscle relaxation, mental images and music to ease your tension.
Biofeedback teaches you to recognize when tension is building in your body. You learn how your body responds to stressful situations and ways to settle it down. During biofeedback, sensors are connected to your body. They monitor your involuntary physical responses to headaches, which include increases in:
Occasional tension headaches usually respond well to over-the-counter pain relievers. But be aware that using these medications too often can lead to long-term daily headaches (medication overuse headaches).
For frequent or severe headaches, your provider may recommend prescription headache medications. Triptans and other types of drugs can stop a migraine attack. You take them at the first signs of an oncoming headache.
Drugs for high blood pressure, seizures and depression can sometimes prevent migraines. Your healthcare provider may recommend trying one of these medications to reduce headache frequency.
Treatment for secondary headaches involves treating the underlying medical condition causing it.
For example, surgery is often needed to correct the underlying cause of secondary cough headache.
You can treat the occasional, mild headache at home with over-the-counter pain relievers. Other self-care treatments for headaches include:
Treating health problems that cause headaches, such as high blood pressure, can eliminate head pain. Recently, there have been several new advancements in our understanding of what causes headaches.
Although researchers are closer than ever before to a cure, at this time, there isn’t a cure for primary headaches. Treatment focuses on relieving symptoms and preventing future episodes.
The key to preventing headaches is figuring out what triggers them. Triggers are very specific to each person — what gives you a headache may not be a problem for others. Once you determine your triggers, you can avoid or minimize them.
For example, you may find that strong scents set you off. Avoiding perfumes and scented products can make a big difference in how many headaches you have. The same goes for other common triggers like troublesome foods, lack of sleep and poor posture.
Many people, however, aren’t able to avoid triggers or are unable to identify triggers. In that case, a more personalized multidisciplinary approach with a headache specialist is often necessary.
Contact your healthcare provider if you or your child has any of the following symptoms or situations:
If your headaches are interfering with your daily functioning or affecting your mood, it’s important to talk to your healthcare provider. If possible, try to write down how you feel when you’re experiencing a headache. Keeping a journal of your headaches and how they make you feel can be helpful when you’re talking to your provider.
The information you give your healthcare provider about your headaches is the most important part of the diagnosis process. By giving your provider as much information as possible about your headaches, you’re more likely to get an accurate diagnosis and treatment plan that will help you feel better.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Do you have headaches that won’t go away? Or ones that come back regularly? Cleveland Clinic’s headache and migraine experts are here to help.
