Lyme disease can develop when an infected tick bites you. The infection can cause a range of symptoms, like a bullseye rash, joint pain and nerve issues. Antibiotics treat Lyme disease. For some people, symptoms linger even after treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
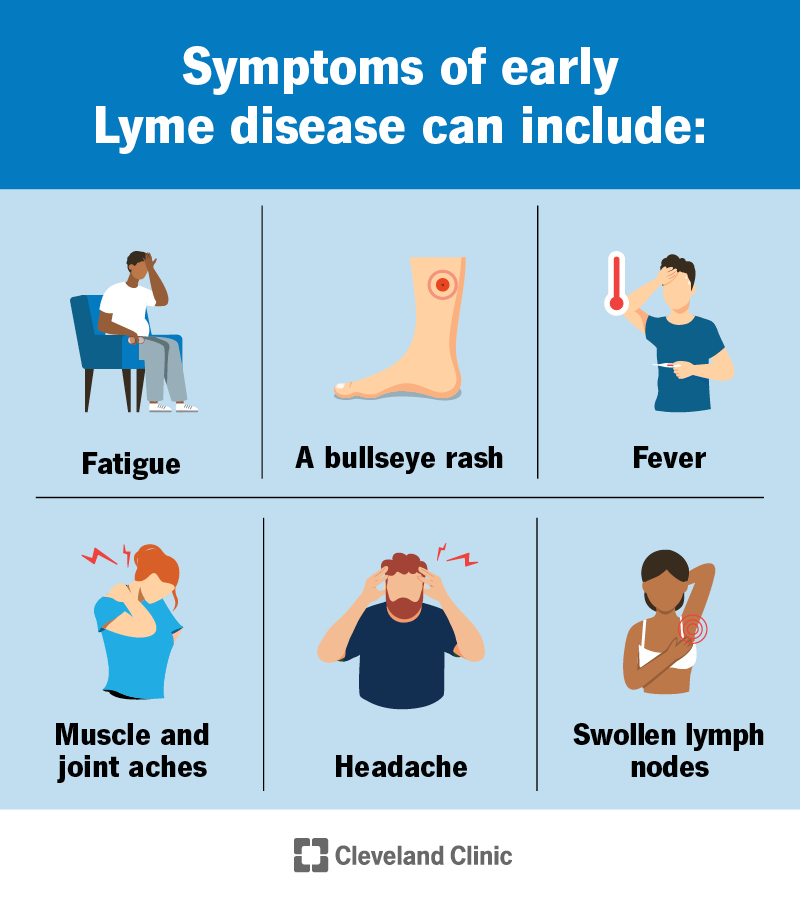
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/lyme-disease-infographic.jpg)
Lyme disease (also called borreliosis) is an infection you can get from the bite of a deer tick. A bacterium called Borrelia burgdorferi causes the infection. Lyme disease is the most common tick-borne infectious disease in the U.S.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Initial symptoms of Lyme disease often include a “bullseye” rash, fever and fatigue. Without treatment, the infection can spread to many parts of your body. It can lead to complications that affect your nervous system, heart and joints.
Ticks are tiny creatures that can do a lot of damage to your health. That’s why you should be aware of where deer ticks live and do everything you can to prevent bites.
Lyme disease can progress through three stages, including:
Early treatment can help prevent the progression to late-stage Lyme disease.
The symptoms of Lyme disease can vary depending on the stage.
Symptoms of early Lyme disease include:
The bullseye rash starts as a small, red spot at the site of the tick bite. This can happen at any time between one and four weeks after the bite. The spot expands in the coming days or weeks, forming a circular, triangular or oval-shaped rash. The rash may look like a bullseye because it appears as a red ring that surrounds a clear center area. It can range in size from a dime to the width of your body.
Advertisement
Not everyone with Lyme disease develops this rash. It appears in about 7 to 8 out of 10 infected people.
Symptoms of the second stage of Lyme disease may include:
Symptoms of untreated late Lyme disease may include:
A bacterium called Borrelia burgdorferi causes Lyme disease. You can get it if an infected deer tick (also called a blacklegged tick) bites you. In general, infected ticks must be attached for more than 24 hours to spread the infection.
Ticks that spread Lyme disease mostly live in wooded areas in the northeastern, mid-Atlantic and north-central United States. Depending on the stage of their life cycle, blacklegged ticks can range in size from that of a poppy seed to a sesame seed. They’re usually black with areas of reddish-brown or white on their backs, depending on whether they’re adults or nymphs
Taking steps to help prevent tick bites can lower your risk of developing Lyme disease.
Untreated Lyme disease can lead to complications like:
Your healthcare provider considers many factors when assessing you for Lyme disease, like:
Many people don’t remember or know that they’ve been bitten by a tick. This is because the tick is tiny, and its bite is usually painless.
Your provider may confirm the diagnosis using a blood test. It checks for antibodies to the bacterium that causes Lyme disease. But it can take several weeks after the initial infection for your body to make enough antibodies for the test to detect.
To be on the safe side, your provider may prescribe treatment without this blood test if:
Advertisement
Antibiotics are the primary treatment for Lyme disease. Common antibiotics include doxycycline, amoxicillin or cefuroxime axetil.
How long you need medicine may vary based on your symptoms or the stage of Lyme disease. For example, you may be on antibiotics for around 10 days for the early stage. If you develop neurological or heart symptoms, you may need to take them for longer. Your healthcare provider will give you specific instructions. Be sure to complete your round of antibiotics.
You may need other treatments to manage symptoms. For example, heart block may require a pacemaker. If arthritis symptoms don’t respond to antibiotics, steroid injections and other therapies may help.
No. You need antibiotics to fight off Lyme disease. Without treatment, the infection can spread in your body and cause complications.
If you feel sick after spending time in areas where ticks might live, you should see your healthcare provider.
If you have a Lyme disease diagnosis and don’t feel better after taking all your antibiotics, contact your provider. This is especially true if you have symptoms like a stiff neck or mental confusion.
Early treatment with antibiotics cures most cases of Lyme disease. According to one study, about 80% of people who get early treatment recover completely. Recovery may be slower for some than for others. Keep in contact with your healthcare provider so they can monitor you.
Advertisement
Untreated Lyme disease may lead to serious health issues. But it’s rarely fatal.
Even after treatment, about 5% to 15% of people may experience lingering symptoms, like pain or fatigue. This is known as post-treatment Lyme disease syndrome (PTLDS). The symptoms don’t mean that you still have an infection. It’s more likely that your body didn’t respond properly to treatment.
More antibiotics are unlikely to help PTLDS. Instead, your healthcare provider will suggest other therapies to manage your symptoms.
You can try to prevent Lyme disease by avoiding tick bites and promptly removing ticks. If you remove a tick within 24 hours, you can greatly reduce your chances of getting the infection.
Researchers are working on a vaccine for Lyme disease. It’s currently in clinical trials. If it’s successful, the vaccine may be another way to help prevent the infection.
If you’re going to spend time in an area that might have ticks, take measures to avoid being bitten. These simple habits can help prevent Lyme disease. If you find a tick on yourself, don’t panic. Remove it carefully and reach out to your healthcare provider to see if you need treatment.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
