Chlamydia is one of the most common sexually transmitted infections (STIs). You can get chlamydia from intercourse, anal sex or oral sex. Because chlamydia often doesn’t cause symptoms, many people who have chlamydia don’t know it and unknowingly infect other people. Regular screenings can help reduce chlamydia’s spread.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chlamydia is a common sexually transmitted infection (STI) caused by bacteria. Chlamydia infections are treatable and curable. However, its symptoms are often unnoticeable. It’s important to receive treatment for chlamydia as soon as possible. Left untreated, chlamydia can lead to serious complications and cause permanent damage to your reproductive organs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Once a person has chlamydia, they can spread it to their partners through sexual intercourse, anal sex or oral sex. Infections can also occur when a person with chlamydia shares sex toys with their partners.
Yes. Sexual intercourse isn’t the only way you can get chlamydia. For example, sharing sex toys with a person who has the infection is another way you may get it.
Anyone who’s sexually active can get chlamydia. The bacteria that causes chlamydia transfers through vaginal fluid and semen. This means anyone who has sex can become infected with chlamydia and infect their partners, too. If you’re pregnant and have chlamydia, you can pass it on to your newborn.
Chlamydia is the most common STI caused by bacteria. About 1.5 million cases of chlamydia are reported each year. The number of infections is likely even higher. Most cases of chlamydia are asymptomatic, which means there are no signs or symptoms of an infection. Many of these cases likely go unreported.
Certain demographic characteristics (like age, sex and race) may make you more likely to get diagnosed with chlamydia. People who are more at risk for chlamydia include:
Advertisement
Higher rates of transmission among certain groups are less about sexual behavior and more about networks and lack of access to STI prevention resources. For example, chlamydia is more likely to spread from person to person within communities that have higher infection rates. And it’s more likely to spread among groups that don’t have easy access to sex education or barriers to STIs like condoms and dental dams.
Chlamydia testing is recommended by the Centers for Disease Control and Prevention (CDC) as part of your regular health maintenance.
Chlamydia infections spread through sexual contact, when vaginal fluid or semen containing the bacteria that causes chlamydia travels from one person to another. Sexual contact includes all kinds of sex, including sex that doesn’t involve penetration or ejaculation. There are lots of ways that the fluids from one person’s genitals can transmit the bacteria that causes chlamydia:
Not all situations involving an exchange of body fluids or intimacy cause chlamydia. You can’t get chlamydia from:
Chlamydia is sometimes called a silent infection because the majority of people (between 50% and 70%) who have chlamydia — regardless of sex — never notice symptoms.
People who do notice symptoms often don’t recognize the signs that they have chlamydia until a few weeks after they’ve been infected. Because chlamydia cases are often asymptomatic, it’s easy to spread chlamydia to someone else without realizing it. And it’s easy to miss out on receiving the treatment needed to prevent the serious complications that can result from chlamydia.
For most people, symptoms of chlamydia show up between one week and three months after unprotected sex. But, it can take longer than three months. Your healthcare provider may learn more about the infection when they diagnose it. For example, a provider may be able to tell that the infection has spread to your fallopian tubes or testicles. It’s important to receive regular testing for STIs if you’re sexually active because you may unknowingly have an infection.
Advertisement
If you do notice symptoms, you’ll likely experience them differently based on if you have a penis or vagina.
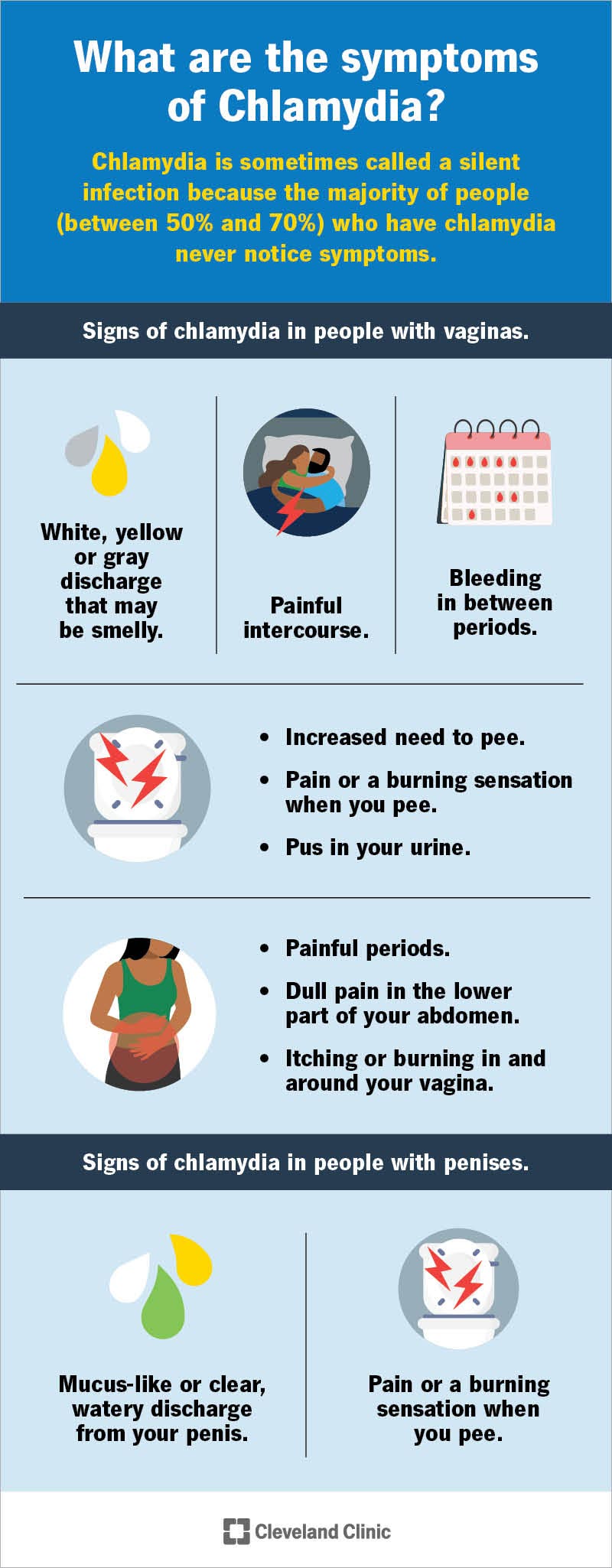
Chlamydia bacteria often cause symptoms that are similar to cervicitis or a urinary tract infection (UTI). You may notice:
Chlamydia bacteria most often infect your urethra, causing symptoms that are similar to nongonococcal urethritis. You may notice:
Chlamydia can affect parts of your body other than your reproductive organs, such as your:
Advertisement
See your healthcare provider immediately if you notice any of these symptoms.
Most people who have chlamydia never notice symptoms. But an unusual discharge from your vagina or penis may be a sign that you have a chlamydia infection. Pain, bleeding or discharge from your bottom can also be a sign of chlamydia.
The most common test for chlamydia is called a nucleic acid amplification test (NAAT). Your provider takes a sample of fluid by doing a vaginal/cervical swab or collecting a urine sample. Then, they send the sample off to a lab to check for the bacteria that causes chlamydia. Your provider may do the test in an office, or they may ask you to do an at-home chlamydia test. Follow your provider’s instructions carefully to ensure you get accurate test results.
Because most chlamydia cases are asymptomatic, it’s important to get screened for chlamydia even if you don’t notice any signs of infection. The CDC recommends that sexually active women who are high-risk for chlamydia get screened regularly. Women more so than men experience the most severe complications from chlamydia. For this reason, women should be screened regularly, too.
You’re considered high-risk if you:
Advertisement
Men should get screened for chlamydia if:
Regardless of your age, reproductive anatomy, or other risk factors — you should discuss your sexual history and sexual activity with your healthcare provider. Your provider is your best resource for offering guidance on how often you should be tested for chlamydia and other STIs.
Chlamydia can be cleared up with antibiotics in about a week or two. But don’t stop taking your medication just because your symptoms improve. Ask your provider about what follow-up is needed to be sure your infection is gone after you’ve finished taking your medicine. Chlamydia infection can recur.
Part of your treatment should also include avoiding sexual activities that could cause you to get re-infected and ensuring that any sexual partners who may be infected also get treatment. You should:
Antibiotics can get rid of your infection, but they can’t reverse any harm the bacteria may have caused to your body before treatment. This is why it’s so important to get screened regularly for chlamydia, to see your provider at the first sign of symptoms, and get treatment immediately if you’re infected.
You should never wait for chlamydia to go away on its own. Left untreated, chlamydia can cause serious harm to your health. If you’re sexually active, you run the risk of infecting others, putting them at risk of experiencing severe complications, as well.
The most common antibiotics used to treat chlamydia infections are:
Make sure you only take antibiotics prescribed by your provider, and take all medications until they’re gone, even if your symptoms improve.
Yes. Chlamydia can be treated and cured. Some sexually transmitted bacterial infections are starting to become resistant to antibiotics, though, and this makes them harder to treat. With this in mind, the best way to fight chlamydia is to prevent infections from spreading.
Untreated chlamydia can put your health at risk. Make an appointment with your provider immediately if you notice any symptoms of chlamydia, and get regular STI screenings to avoid complications later.
Untreated chlamydia can cause:
Untreated chlamydia can cause:
Untreated chlamydia can spread to your bloodstream, which:
You should start to feel better within a week after you begin taking antibiotics. Be sure to continue taking your antibiotics until they’re gone, even if your symptoms improve.
Don’t have sex with anyone (intercourse, anal or oral) for at least seven days from when you began treatment. This gives the medication time to work so you don’t infect your sexual partners. Once treatment is over, you should still practice safe sex and get tested for STIs as a part of your regular health maintenance.
With treatment, chlamydia should go away within a week or two, however, the test may remain positive for 4 weeks after treatment. It’s important to take all antibiotics to fight the infection. Don’t have sex during treatment, or you could get reinfected.
The only way to avoid getting chlamydia is to abstain from having vaginal, anal or oral sex with someone who has a chlamydia infection. And be sure that sex toys that carry the bacteria don’t come in contact with your genitals.
It’s not always possible to know if a current or potential partner has chlamydia, though, especially since many people with chlamydia never notice symptoms. With prevention in mind, it’s a good idea to make safer sex practices a regular part of your sex life:
When it comes to chlamydia, it’s a good idea to be proactive. Speak with your healthcare provider about your risks of infection. Make a plan to get screened regularly for STIs based on your provider’s recommendations for how often you should be tested. Make an appointment with your healthcare provider if your partner tests positive for chlamydia or if you notice any signs or symptoms that you may be infected.
Chlamydia doesn’t always have a smell. But one of the symptoms of chlamydia is an unusual vaginal discharge that has an unpleasant odor.
You can get chlamydia if your partner had vaginal, oral or anal sex with someone who was infected and then had sex with you. People in relationships may have different ideas about what kinds of sexual contact counts as “cheating,” and this miscommunication can lead to infections. Communicate honestly with your partner about what sex you’re having and what sex they’re having. Practice safer sex to reduce your risk of catching chlamydia, and get regularly screened to be sure.
Symptoms of chlamydia can take weeks, months or years to start. Often, you have no symptoms and don’t know you have it. This means you may have gotten chlamydia from previous sexual partners. If you’ve had many sexual partners and have unprotected sex, it’s a good idea to get tested for chlamydia.
It can be embarrassing to talk about anything sex-related with your healthcare provider, including STI prevention. But your sex life is an important part of your health that your provider needs to know about to care for you. Not getting the treatment you need for chlamydia can pose serious risks to your health. Speak with your provider about getting regularly screened for chlamydia and other STIs to reduce your risks of complications. Practice safer sex to prevent the spread of chlamydia.
Don’t ignore sexually transmitted infections. Cleveland Clinic experts will treat them confidentially and quickly in a judgment-free environment.

Last reviewed on 02/06/2023.
Learn more about the Health Library and our editorial process.