A tracheostomy is a hole your surgeon makes through your neck and into your trachea (windpipe) to help you breathe. This new passage delivers oxygen to your lungs by bypassing your nose, mouth and throat. You might need a tracheostomy if you have an obstructed upper airway. A tracheostomy may be temporary or permanent.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
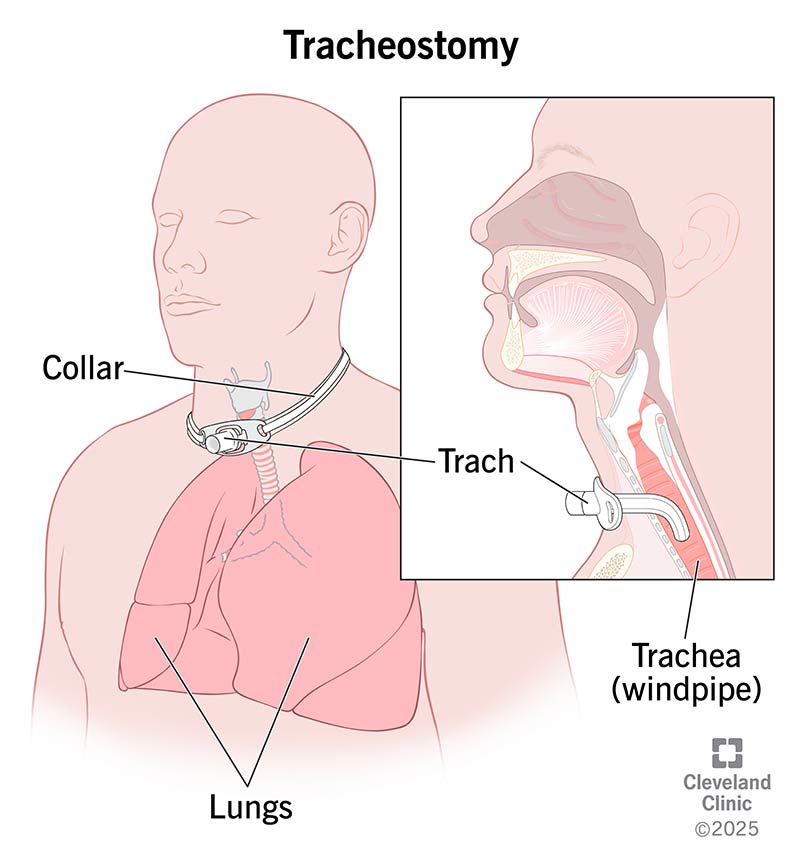
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/tracheostomy)
A tracheostomy is an opening a surgeon makes through your neck and into your trachea (windpipe). A tracheostomy tube, or trach (pronounced “trake”), goes through the hole and into your windpipe to help you breathe. The actual procedure to create the tracheostomy (opening) is called a tracheotomy. But most healthcare providers use these terms interchangeably.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A tracheostomy allows you to get air through your neck when you’re having trouble breathing through your mouth and nose. You may need a tracheostomy if you:
Depending on your situation, a tracheostomy might be temporary or permanent. It’s usually an elective procedure (one you schedule and prepare for). But sometimes, it’s an emergency treatment.
Your healthcare provider will tell you how to prepare for an elective tracheostomy. If you’ll be under general anesthesia, you may need to fast or stop taking certain medications for several hours before your appointment.
You’ll also need to pack a suitcase to bring with you. Most people need to stay in the hospital for a few days to a few weeks after surgery. Your provider may tell you to bring:
Advertisement
Open tracheotomy surgery takes place in an operating room. First, you’ll likely get general anesthesia so you’re asleep. Once you’re comfortable, your surgeon will create an incision (cut) in your neck, just below your Adam’s apple. This incision will go through the wall of your windpipe. Next, your surgeon will gently widen the opening enough to fit a tracheostomy tube inside.
Once the tube is in place, your surgeon will secure it with a tracheostomy collar that goes around your neck. Your surgeon may also place temporary stitches. This keeps the tube in place during your recovery.
If you’re unable to breathe on your own, your surgeon will hook the tracheostomy tube up to a ventilator.
A percutaneous tracheostomy is a newer form of the procedure. It often happens at your bedside in the hospital. Instead of making cuts to access your trachea, a surgeon inserts a needle to create a hole in your neck and windpipe. They’ll insert a wire to guide a small plastic tube (catheter) inside that they’ll use to widen the opening.
Then, they’ll insert the tracheostomy tube.
A tracheostomy helps you get air when you’re unable to breathe through your mouth and nose. Compared to intubation, it’s more comfortable. It also helps many people transition from being on a ventilator to breathing on their own.
Still, like any surgical procedure, there are some risks associated with tracheostomy. Possible complications include:
Keeping your tracheostomy tube clean and following your healthcare provider’s instructions can reduce your risk of complications.
After your tracheostomy, your medical team will watch your progress to ensure a successful recovery. Until you can meet with a speech-language pathologist (SLP), you’ll communicate through writing.
Your healthcare provider will give you instructions before you leave so you know how to take care of yourself and your tracheostomy tube at home.
Advertisement
On average, a tracheostomy takes about two weeks to fully heal. It’s common to feel neck soreness during this time. It may take a day or two to get used to breathing through your trach tube.
If your tracheostomy is temporary, your healthcare provider can remove your trach tube once your airway is open. The removal process is called decannulation. Sometimes, the hole closes on its own within a few weeks. Or you may need a procedure to seal it. Afterward, most people have a tiny scar where their incision was.
Whether your tracheostomy is temporary or permanent, your healthcare provider will give you instructions about adjusting to life with a trach.
Before leaving the hospital, you’ll receive instructions about how to care for your tracheostomy tube at home. Typically, you’ll need to clean your tracheostomy tube at least twice a day. You’ll also need to return to your healthcare provider’s office so they can change out the tube. Your provider will tell you how often your tube will need to be replaced.
You can speak with a tracheostomy after you’ve had some time to heal, but it’ll take practice. You can speak by covering your tracheostomy hole with a finger and forcing air out through your mouth. A speech-language pathologist (SLP) can teach you how to do this.
Advertisement
There are also speaking valves that can help you talk. These allow you to speak without using your finger to cover your tracheostomy hole.
Be patient with yourself as you try to talk. At first, speaking may make you feel winded. Take your time and use writing instead if you’re feeling exhausted. Ask your SLP about resources or devices that can help you communicate.
It may take a while to eat and swallow like you’re used to. At first, you may need to receive nutrition through an IV or feeding tube. A speech-language pathologist can teach you exercises to help you swallow so you can eat more comfortably.
Get as much rest as possible during recovery. Your healthcare provider will tell you how much activity is acceptable. Generally, it’s a good idea to do a brief walk each day. Movement can help keep your lungs clear and prevent constipation. But it’s important not to overexert yourself.
Contact your healthcare provider right away if you:
Advertisement
You should also reach out to your provider if your trach tube changes position or slips out of place.
A tracheostomy can be a form of life support. Your surgeon may attach your tracheostomy tube to a ventilator if you can’t breathe on your own. Depending on your situation, a trach may help you transition from using a ventilator to breathing on your own.
You may need a tracheostomy in the short-term, long-term or permanently. But for most people, a trach is temporary.
Hearing that you need a tracheostomy can feel scary and uncertain. But most people who have one learn to breathe, eat and speak quite well with the help of their care team. Talk to your healthcare provider about how to adapt after a tracheostomy. Whether you need a trach tube temporarily or permanently, you can still lead a fulfilling life with a tracheostomy, doing the things you enjoy.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic has a specially trained team for tracheostomy care and removal. Our compassionate healthcare providers keep you safe, comfortable and prepared.
