Gastrectomy is stomach removal surgery. Total gastrectomy removes your entire stomach. Partial gastrectomy removes part of your stomach. You may need this operation to treat stomach (gastric) cancer, severe (Class III) obesity or other stomach conditions that haven’t responded to less invasive treatments, like medication and lifestyle changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
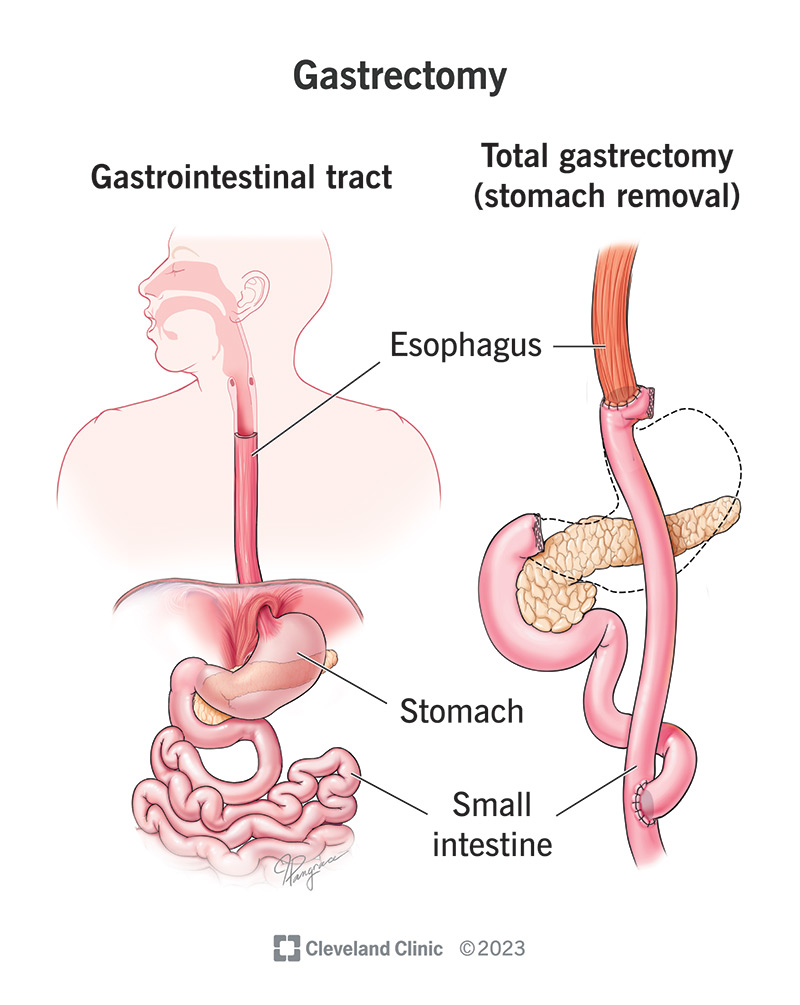
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/gastrectomy.jpg)
A gastrectomy is a surgery that removes all or part of your stomach. Your stomach is your digestive system’s food reservoir. It allows you to store and break down the food you eat before it travels to your small intestine, which absorbs nutrients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But if you develop a condition like stomach (gastric) cancer, your stomach can cause more harm than good. In that case, you may need a gastrectomy. Although a gastrectomy changes your digestive system, you can live (and eat) without a stomach.
There are two main types of gastrectomy:
Gastrectomy most commonly treats stomach cancer. You may need a total or partial gastrectomy to cure the cancer (eliminate it) or prevent it from spreading. Gastrectomy can also be palliative when the cancer isn’t curable. This means the surgery relieves cancer symptoms, like stomach bleeding and pain.
Healthcare providers sometimes use gastrectomy to treat other conditions. It may be a last resort when less invasive treatments like medicine and lifestyle changes haven’t helped enough.
Advertisement
Gastrectomy treats:
You may choose to have your stomach removed to prevent hereditary diffuse stomach cancer. You’re at high risk of developing this cancer if you inherit a mutation (error) in a gene called CDH1 from a biological parent. This cancer is nearly impossible to detect early when treatments work best. If you have this mutation, your healthcare provider may recommend total gastrectomy.
During surgery, your surgeon removes all or parts of your stomach. They reconstruct your digestive system so you can continue to receive nourishment.
Your healthcare provider will:
Advertisement
It can take up to five hours, depending on the type of gastrectomy and whether it’s open surgery or laparoscopy. It’s a major operation that requires lots of time and care on the part of your care team.
You’ll need to remain in the hospital for up to two weeks so your healthcare team can monitor you. They’ll ensure you’re getting the nutrition you need. They’ll also ease you into eating solid foods. They’ll work with you to monitor your pain levels and provide pain medicines as needed.
While everyone’s journey is different, you can expect some typical phases as you start recovering in the hospital:
Your care team will also advise you on wound care. For example, you may need to stick to sponge baths instead of baths or showers until your wound heals.
A gastrectomy can be a lifesaving procedure that cures or slows the spread of stomach cancer. When used as bariatric surgery, it can prevent potentially life-threatening complications associated with Class III obesity. It can also improve your quality of life by eliminating symptoms.
Advertisement
As with any surgery, complications include infection, being allergic to anesthesia and blood clots. You may need to wear compression socks after surgery to reduce your risk of clotting.
Complications unique to gastrectomy include:
Advertisement
Tell your healthcare provider about any complications you’re experiencing. It’s important to attend all follow-up appointments so they can ensure you’re healing without issues.
Gastrectomy is a major surgery that requires months — not weeks — to heal. It may take up to two months to heal from the surgery. Regaining your energy levels and getting used to your new eating habits may take three to six months or even longer. Be patient with yourself as your body repairs itself and adjusts to the changes in your digestive system.
It may take a month or more before you can safely drive yourself. Ask your healthcare provider what’s safe for you.
Plan to take several weeks or even a few months off work, depending on your job type. Some people work remotely at first before returning to the office. Others resume part-time work before transitioning to full-time. Ask your healthcare provider what to expect based on your situation.
You can live a healthy, normal life without a stomach. Still, you’ll have to find a new normal regarding the types of food you eat and how often you eat. Foods you ate before without issues may make you feel sick after a gastrectomy. You’ll likely need to find a new balance to ensure you get enough nutrients — without eating so much that you’re straining your digestive system.
Here are some tips to help you transition into your new normal post-surgery:
Keep all follow-up appointments with your healthcare provider so they can ensure you’re healing as you should. In the meantime, alert your provider if you’re experiencing new symptoms or if any of the following symptoms are worsening:
See your provider if you’re noticing signs of an infection like a fever or any of the following at the surgical site:
Your healthcare provider will only recommend a gastrectomy if the benefits outweigh the risks and stresses of adjusting to a changed digestive system. Getting used to life after this surgery requires time and patience. After all, for most of us, eating is one of the simplest and most enjoyable activities we experience each day. Having to be more deliberate about food and drink choices requires some adjustment. Still, many people who’ve had this surgery live full and healthy lives.
Ask your provider about what to expect during and after recovery. Understanding how your surgery may change your routines in the short and long term can help you approach the idea of a gastrectomy with more confidence.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have obesity and losing weight is an uphill battle, Cleveland Clinic experts can help you decide if bariatric surgery is an option.
