Oral appliances for sleep apnea work by pulling your jaw or tongue forward while you sleep, opening your airway. Your healthcare provider may recommend an oral appliance to treat obstructive sleep apnea if you can’t use a CPAP machine. Types include mandibular advancement devices and tongue-stabilizing devices.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
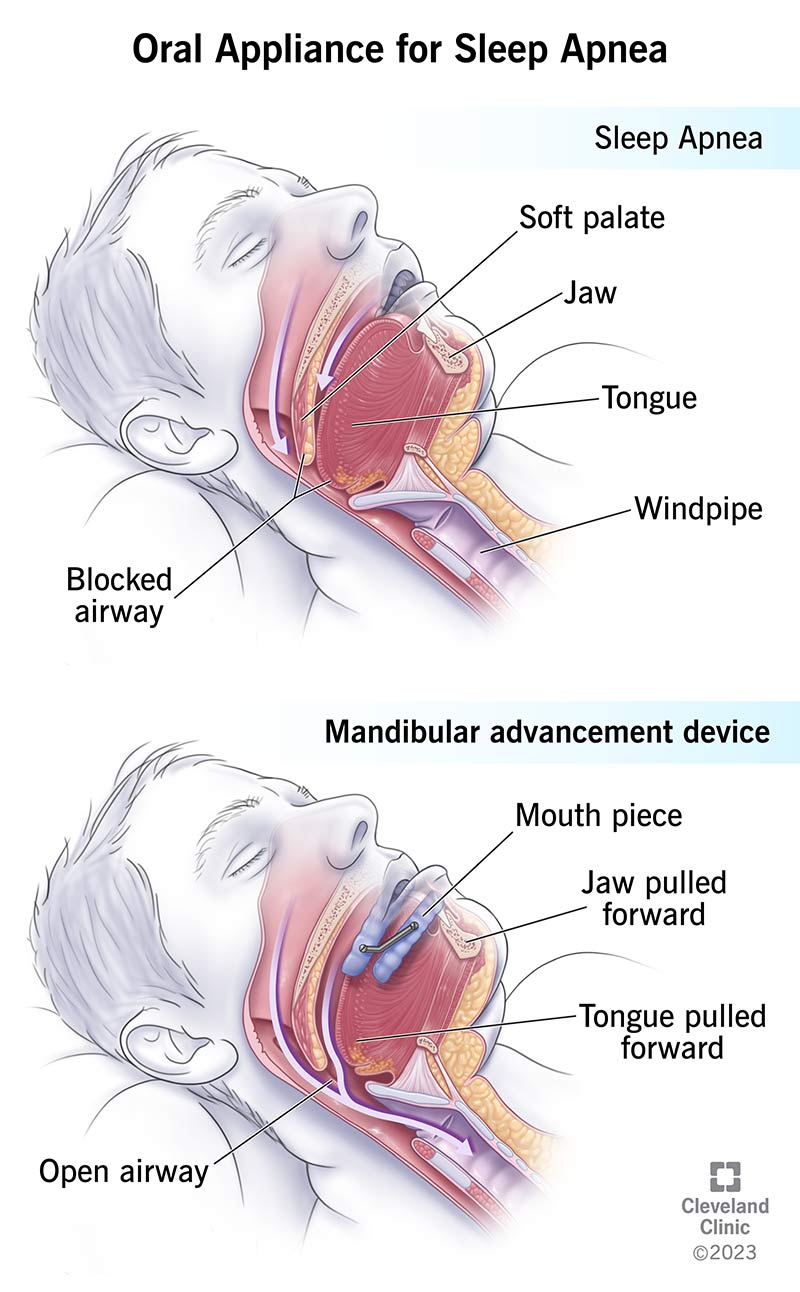
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/oral-appliance-for-sleep-apnea)
Oral appliances for sleep apnea are dental devices, or mouthpieces, that you wear in your mouth to keep your airway open while you sleep. Healthcare providers use them to treat obstructive sleep apnea (OSA).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With OSA, your upper airway is blocked partly or completely when you’re sleeping. The reduced airflow triggers your brain to wake you up just enough to keep breathing. The cycle of restricted airflow, waking and falling asleep again, continues throughout the night. These episodes stop you from sleeping soundly and prevent your vital organs from getting enough oxygen. Untreated, OSA can lead to serious health conditions and is potentially fatal.
Oral appliances, also called oral appliance therapy, treat OSA. They hold your mouth in a position that makes sure you get enough airflow. They help you breathe better and reduce how often OSA wakes you up.
There are two main types of dental appliances for treating OSA: mandibular advancement devices (MADs) and tongue-stabilizing devices (TSDs).
Mandibular advancement devices (MADs) are the most common oral appliance for treating OSA. They’re also called mandibular advancement splints, mandibular advancement appliances or mandibular repositioning appliances.
MADs work by pulling your lower jaw (mandible) forward. Moving your jaw forward also pulls your tongue forward, creating more space for airflow in the back of your throat. MADs fit over your teeth. Most come in two parts, one for your top teeth and one for your bottom. Screws, hinges and adapted rubber bands connect the top and bottom, allowing you to pull the lower part of the device that controls your jaw forward. Others have independent interchangeable arches.
Advertisement
MADs vary in terms of:
Tongue-stabilizing devices (TSDs) are also called tongue-retaining devices. They treat OSA by pulling your tongue forward using suction. A suction bulb on the device holds your tongue in place while you sleep. The tip of a TSD stays outside of your mouth. Like MADs, TSDs open your airway by moving the base of your tongue forward.
TSDs aren’t as popular as MADs, but they may be an option for people with OSA who want to try an oral appliance but can’t use MADs. For example, people whose teeth aren’t strong enough to hold a MAD in place may use a TSD instead. These are also available over the counter.
The most effective oral appliances are custom-made to fit your mouth. You can buy oral appliances without a prescription, including “boil and bite” models that make an impression of your teeth. These types may provide benefits, but research shows that custom-made oral appliances offer the best results for OSA.
Oral appliances pull the base of your tongue forward, creating more space in the back of your throat. Some types latch onto your tongue and pull it forward. Most pull your lower jaw forward while your tongue remains in place.
You put the device in before you go to sleep and wear it throughout the night. You remove it in the morning when you wake up.
Oral appliances work best for people with mild to moderate OSA who can’t use a CPAP (continuous positive airway pressure) machine. A CPAP is a machine that attaches to your airway through a tube and mask you wear at night that sends pressurized air through your airways, keeping them open.
While CPAP is the best treatment for improving airflow for people with sleep apnea, many find it challenging to use night after night. Over time, they stop. Oral appliance therapy isn’t as effective as CPAP, but it does improve symptoms in some people.
Other people use oral appliances and CPAP together. For example, you may use a CPAP machine at home but an oral appliance when traveling. You may use an oral appliance with a CPAP machine to decrease the amount of pressurized air you’re getting from the CPAP.
Oral appliances aren’t for everyone, including:
Advertisement
You’ll need a sleep study to diagnose your OSA. If your sleep specialist decides an oral appliance is a good option, you’ll need a referral to a dentist.
To fit you for a MAD (the most common type of oral appliance), the dentist will:
The dentist may recommend you have a sleep test after you get your MAD to see how the appliance is working. Based on the results, you may need further adjustments to your appliance.
It takes about two to four weeks to adjust. It may feel odd at first to have a mouthpiece when you sleep. Try wearing it for only a few hours at first and gradually extending how long you have it in. For most people who use them, wearing an oral appliance eventually becomes part of their nighttime routine.
You may notice side effects during the first week or two while you’re adjusting. Symptoms usually improve once you get used to wearing your appliance.
Advertisement
Short-term side effects include:
Long-term side effects are uncommon with a properly fitted appliance. When issues occur, they include:
Visit a dentist regularly so they can check for changes in your dental health and make corrections as needed. They’ll also ensure your device remains in good shape. Bring your device with you to all future dental appointments.
Oral appliance therapy:
Your response depends on the shape of your mouth and how severely OSA affects you. Some people with mild to moderate OSA find an oral appliance completely resolves their symptoms. Other people don’t notice an improvement and need different treatments.
Your dentist will explain all the potential benefits. They can explain the pros and cons of using an oral appliance for obstructive sleep apnea.
Advertisement
Oral appliances help people with obstructive sleep apnea (OSA) get a better night’s rest. They can eliminate or reduce excess snoring, too. Ask your healthcare provider about using an oral appliance if you’re finding it hard to use a CPAP machine consistently. In some cases, you may need to stick with a CPAP. Talk to your healthcare provider about an oral appliance. They’ll suggest one that’s the best fit for you and your specific OSA symptoms.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Obstructive sleep apnea can keep you from the getting the good night’s rest you need. Cleveland Clinic’s experts can create a treatment plan that helps.
