
Kashton “Kash” Wanner was born 14 weeks early on Jan. 8, 2024, at Cleveland Clinic. Weighing just 1.3 pounds, Kash was diagnosed with bronchopulmonary dysplasia, which can include a severely narrowed airway. This condition and other complications kept him in the Neonatal Intensive Care Unit (NICU) for 268 days.
“Each time they took the tube out to let him breathe on his own, he wasn’t ready, and they would put it back,” his mother, Stephanie, says. “He’s an active baby and kept pulling out the tube. This went on for about four months. They finally sat me and his dad down and said that he would either need a tracheostomy, or he would have to be sedated and on the tube 24/7.” The procedure would create an opening in his windpipe, allowing air to pass directly into his lungs through a tube that Kash would be unable to remove. “We did the procedure in May, and after that, he thrived. He also wasn’t able to feed from bottles, so he has a feeding tube in his stomach.
On Sept. 23, 2024, Kash was transferred to Cleveland Clinic Children’s Hospital for Rehabilitation, where he ultimately reached 13 pounds while achieving normal developmental milestones. By June 5, 2025, the day he was discharged, Kash was 16 months old and able to walk out of the hospital. The rehabilitation team who helped him grow and thrive ensured that both he and his family were ready for their next steps.
Kash was happy and excited to join his parents, Stephanie and Anthony, and four big brothers, Antonio, Zayden, Kingston and Anthony Jr., at home. This was a new home not only for Kash, but also for them. The family had moved out of the house where they lived for 11 years and into one that could accommodate his medical equipment and round-the-clock nursing care. Although taking care of Kash is complex, Stephanie, says, she and Anthony were well-trained by the Hospital for Rehabilitation team.
“While Kash was in the hospital, we had time to get an education there, which we finished not long before he was discharged,” Stephanie says. “He has the trach and a nose cap we have to put on. He’s not attached to machines, except for if he gets sick and needs a tiny boost of oxygen. For us, it was like getting a medical degree. We worked alongside the respiratory therapists, including a lot of training with Meredith Clement, who became like family to us. Once they signed us off on the tracheostomy care, our biggest hurdle was finding nurses to come to our home.”
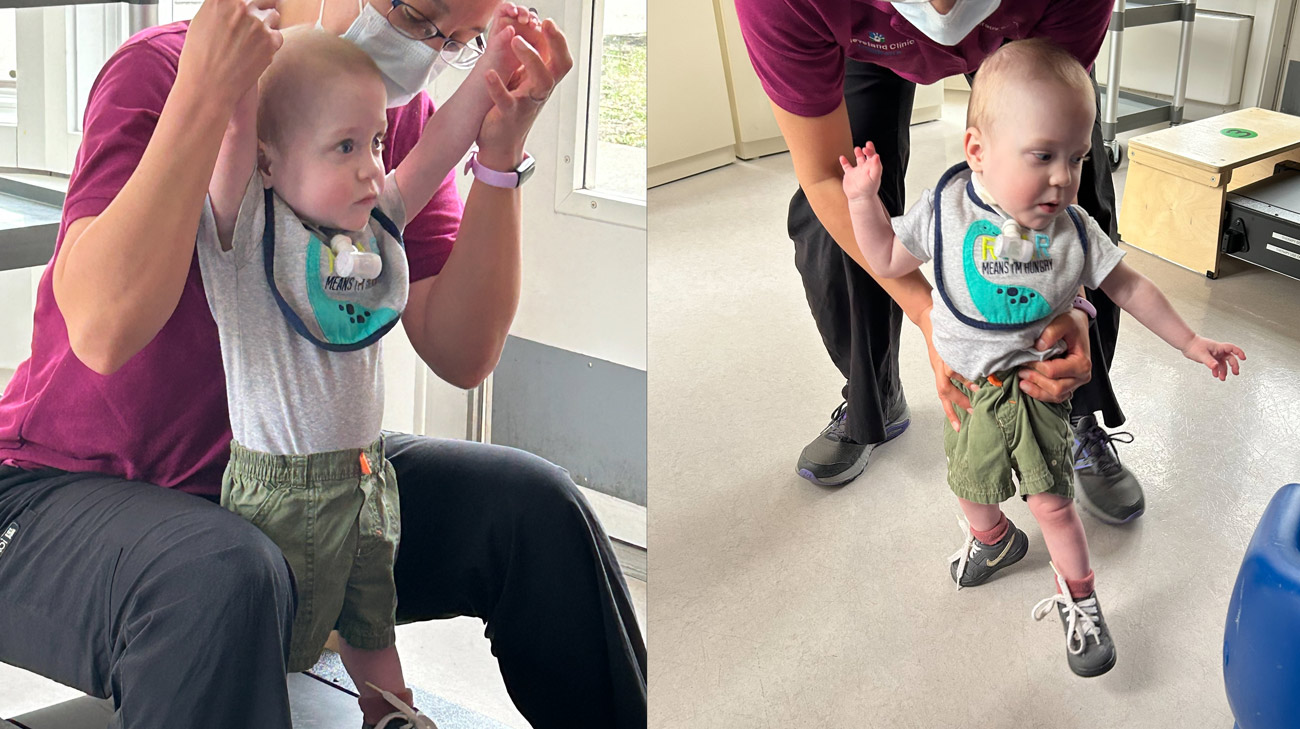
Kash walks with physical therapist Naomi Diaz-Hunter, one of the many Children’s Rehab Hospital caregivers who helped Kash thrive and ensured that both he and his family were ready for their next steps.
Helping the family along the way were Michelle Marks, DO, Medical Director for the Children’s Rehabilitation Hospital and a team of physicians; Soniqua Turner, MSSA, pediatric inpatient social worker; respiratory therapist Meredith Clement, RRT; and Nurse Practitioner Christine Halishak, CPNP, AC/PC. The team also includes a dietitian, occupational, physical, recreational and music therapists, and a speech-language pathologist.
“Christine and I work very closely with patients, supporting them medically throughout their journey,” Dr. Marks says. “Kash came to us last summer pretty severely affected by his respiratory status. He was able to go home with ventilator support only overnight as needed. When he arrived, his development was significantly delayed. When he went home, he walked out. The hope is that as he continues to grow, he will be able to come off of full respiratory support at some point.”
Much of what allows a patient to go home safely revolves around training family members, says Meredith Clement. “As a respiratory therapist, the biggest part of my job is to teach them how to take care of a child with a tracheostomy and ventilator, and the treatments with that,” she says. “We try to structure training around when the families can come in, working with their schedules. It takes literally months to learn all the information about a trach. For Kash’s family, they had other kids at home and were only able to come in on Saturdays. We scheduled 30 minutes to an hour every Saturday. Before they took Kash home, they had to be able to show me that they could manage his trach. I had to be sure they understood how critical this was and that they were comfortable replacing it if it came out. Keeping something like that in place for an active 1-year-old is hard. In a hospital setting, we can’t let him crawl around on the floors like he does at home, for instance. And he has four big brothers. It’s a house full of boys bouncing all over the place.”
From the time patients leave the ICU, the hospital team’s goal for most is to get them home. “I help coordinate this,” Christine Halishak says. “With Kash, there were issues regarding getting him off the ventilator. Working as a team, we did a test of his airway that showed there was a lot more pressure than there should be, a 90% blockage. Then, the plan became letting him gain weight, grow and go home with his airway pretty much closed. He would need therapies and nursing support. We came up with a plan for around-the-clock care, with a team that knows how to troubleshoot. His parents also had to be taught what to do if his airway tube comes out, how to put a new one in.”
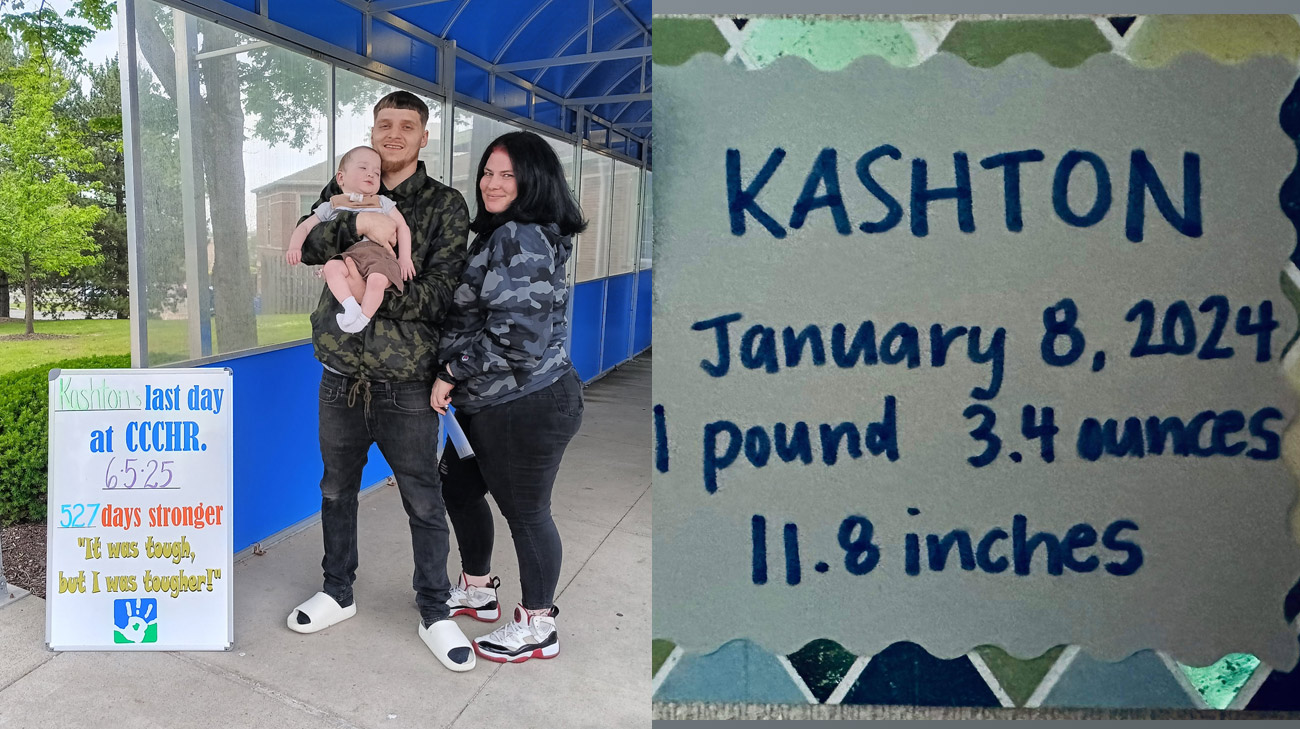
Kash with his parents on the last day of his treatment at Cleveland Clinic Children's Rehab Hospital.
The team also works with medical subspecialists from other departments at Cleveland Clinic, including pulmonology, neurology and endocrinology, as well as the Pediatric Center for Airway, Voice and Swallowing Disorders. “We have family meetings every other week, to discuss what is happening and what we are anticipating,” Christine says.
Social Work is critical in helping patients make the transition from hospital to home. “My primary role is to create a plan for families before they leave the hospital, arranging their training and helping to find the additional nursing care they will need,” Soniqua Turner says. “Kash’s mom and I worked together. I am a needed support to families because this can be a long, drawn-out process, both mentally and emotionally taxing.”
She addresses complex needs that are specific to patients’ situations. In Kash’s case, “he has a critical airway that is very small, and it was a concern for a while whether it would be safe for him to go home,” Soniqua says. “But all of our specialists agreed that it was OK, and his parents were very consistent and on top of their education. From the very beginning, they asked, ‘What do we need to learn?’ The majority of my job is getting the parents in for their education and to help them become comfortable with their child’s care.”
The hospital team addressed many of their greatest challenges, Stephanie says. “They are amazing. It’s one of the best places I’ve ever seen, helping us deal with things I couldn’t handle. Soniqua helped me and the kids when Anthony was getting training and trying to find us a better house. We worked with nursing, respiratory therapy, social work, physicians. If it weren’t for Kash’s therapy teams, he wouldn’t be where he is. They taught him so many things. He’s so advanced because of them, including talking even around the trach. He says, ‘Mama, Daddy,’ and shakes his head ‘yes’ or ‘no.’ His progress is a true testimony of what faith and a team do. Cleveland Clinic took a really scary situation and helped us through it to where we were calm and understood. They made us feel comfortable and confident in what we were doing, and they gave us choices. Kash would light up whenever he saw them.”


