
Each week, Rand Laycock’s hands guide dozens of musicians in a symphony orchestra. For more than four decades, he’s been the director and conductor of the group in Parma, Ohio. The 70-year-old retired music teacher, who started playing the trumpet in fifth grade, hasn't allowed a Parkinson's diagnosis just before his 60th birthday to slow him down.
“When I was diagnosed 11 years ago, my doctor at the time told me this wasn’t a death sentence, and there would be advancements over the next few years to help with my treatment. And here I am today with adaptive deep brain stimulation – something we didn’t even know about at the time,” says Rand of Olmsted Falls, Ohio.
Rand learned he had Parkinson’s disease after going to the doctor for a twitch in his thumb. He started on a regimen of medications, but his symptoms progressed over the years.
“About eight years in, I started experiencing more tremor in my right hand. This was daily and seemed to get worse if I was anxious or nervous. The tremor would really start to be pronounced if I had a deadline coming up for something with the orchestra,” says Rand, who also started experiencing dyskinesias, which are involuntary movements that result as a complication from long-term use of certain Parkinson's medications.
Not being able to control his symptoms with medications alone, Rand learned about deep brain stimulation (DBS) from Michal Gostkowski, DO, a neurologist at Cleveland Clinic. Described as a pacemaker for the brain, DBS involves implanting a device to deliver electrical currents to specific parts of the brain that control movement. This stimulation helps to modulate the abnormal brain signals that cause Parkinson’s symptoms.

Following DBS surgery and the programming of his device, Rand says he noticed immediate improvements in his Parkinson’s symptoms. (Courtesy: Rand Laycock)
In May 2024, Rand moved forward with DBS. He first underwent surgeries to insert the stimulation leads and implant the stimulator battery, which were performed by neurologist and neurosurgeon Sean Nagel, MD. He then activated and set up his device with programmer Erica Hennigs.
“When it comes to programming the device, we try different settings at first. We then adjust those during follow-up visits as we learn more about how his symptoms are being controlled,” says Erica.
Rand saw success with DBS for nearly a year, and then he learned about a new advancement called adaptive deep brain stimulation (aDBS). Patients, like Rand, who received the specific device that supports aDBS can use the technology if their care team were to determine it would be beneficial in further managing their symptoms.
“Traditional DBS gives the same stimulation to the brain 24 hours a day. What makes aDBS different is it can adapt and fine tune the stimulation in real time. By tracking a certain frequency in the brain, it can increase or decrease the stimulation as needed to better control symptoms,” says Dr. Gostkowski.
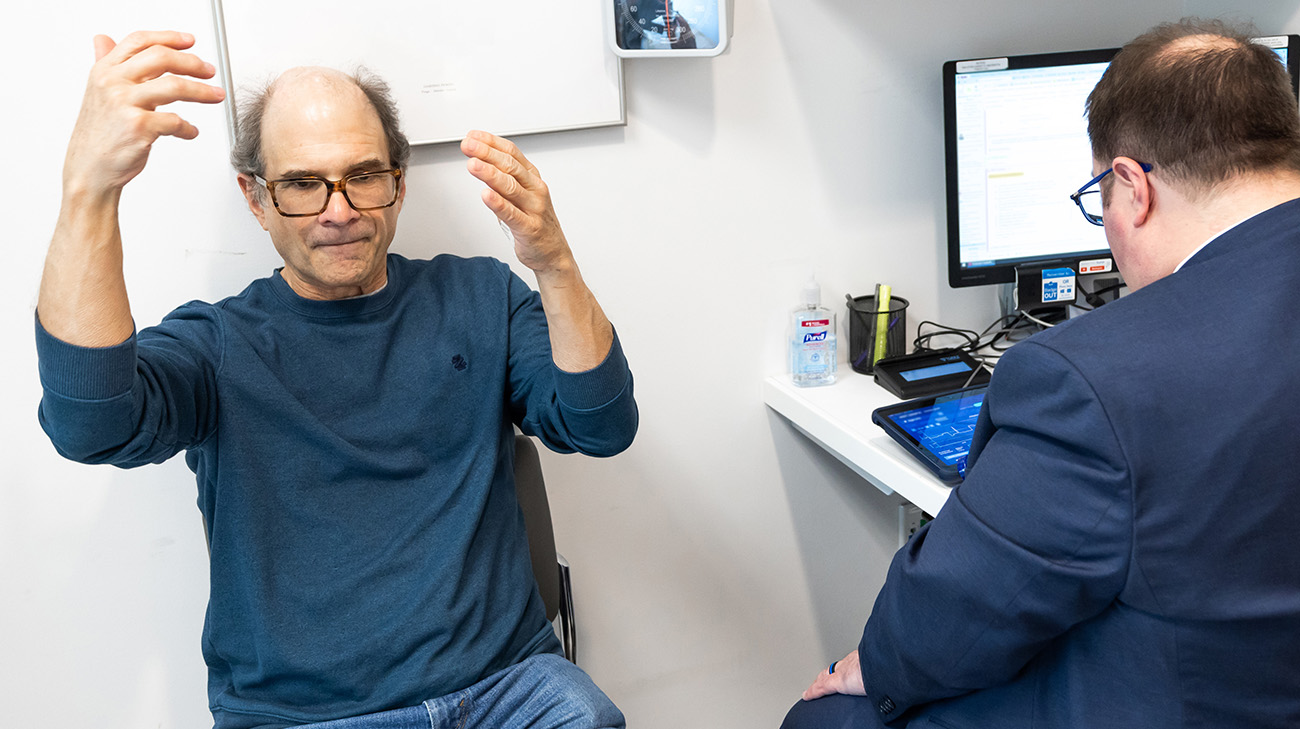
Rand with Dr. Michal Gostkowski at a follow-up appointment. As Rand made the motions he traditionally uses while conducting, aDBS allowed his device to adjust the stimulation as needed in real time. (Courtesy: Cleveland Clinic)
Although not everyone with DBS needs this adaptive technology, Rand was a good candidate for it because his symptoms fluctuated throughout the day. In response, aDBS would be able to automatically increase the stimulation as Rand’s Parkinson’s medications wore off to help prevent tremors. In turn, it could automatically decrease the stimulation when the medication is active to help with dyskinesia.
“Since Rand’s a music conductor, fine tuning with aDBS would reduce the risk of him experiencing tremors if his medication were to wear off in the middle of a concert or performance,” says Erica.
Since his overall experience with DBS had been positive, Rand says he was eager to try the new adaptive technology. “It sounded like it would make my life simpler – not having to worry about adjusting my device settings and medications as frequently.”

With aDBS, Rand says he can focus more on conducting and less on managing his symptoms. (Courtesy: Cleveland Clinic)
In March 2025, Rand started using aDBS. Since his current device was able to support the new adaptive technology, it was just a matter of working with Erica to update the settings. As the system gathers more data regarding Rand’s Parkinson’s, he will continue working with Erica to refine the aDBS for even better symptom control.
“My tremor is almost all gone, except if I experience extreme anxiety or stress – and my dyskinesia is pretty well under control. My symptoms are minimal compared to the way they were, and a lot of that is due to the adaptive deep brain stimulation,” says Rand.
As his symptoms continue improving, Rand looks forward to his 47th year of conducting as well as spending time with his wife, two children and granddaughter. Rand and his care team hope raising awareness about DBS and aDBS can help others who may be candidates for these treatments.

Throughout his health journey, Rand has not only been supported by his care team but by his family as well. (Courtesy: Rand Laycock)
“We still find patients and even neurologists who don’t know about DBS. If you have Parkinson's, it’s worth talking to your doctor about whether DBS or aDBS could help manage your symptoms. These treatments work well and can improve your quality of life,” says Dr. Gostkowski.
Rand adds, “I know the thought of brain surgery can be intimidating, but it’s a life-changing procedure that allows you to become your own self again.”
Related Institutes: Neurological Institute

