
When River Kelly was born at Cleveland Clinic on Feb. 3, 2022, she was diagnosed with a genetic condition called CHARGE syndrome. It affects many areas of River’s body and led to a rare congenital heart defect in which both of her major heart arteries were connected to the right ventricle.
At 3 months old, River had a procedure to place a shunt that helped her heart pump blood to her lungs. At 6 months old, she had another surgery to repair the defect.
“CHARGE not only affected her heart but also left her hard of hearing and caused a large coloboma – a hole – in her left eye,” says her mother, Ashley Kelly.
Before River’s heart repair surgery, she needed a tracheostomy to open her airway. That’s when her family began working with Cleveland Clinic’s Pediatric Center for Airway, Voice and Swallowing Disorders (PCAVS). The team took care of River for the eight months that she was in the hospital.
“They were always checking on her,” Ashley says. “They became almost like our second family. And when she came home in September, I could always call them, and they would respond by the end of the day.”
Ashley was no stranger to pediatric medicine, herself having been a Cleveland Clinic EKG technician who worked with pediatric cardiologists. “I knew most of them before having River,” she says. She also had worked in Cleveland Clinic’s coronary ICU. However, having her own child on the receiving end of this care was a different experience, she says.
“With PCAVS, especially, from the beginning, it wasn’t just about River,” she says. “It was about all of us. The social worker would ask, ‘How are you?’ She would ask about the family and our other kids. When my husband went to Army boot camp, they asked us, ‘How can we help you?’ And they never doubted River. It was always, ‘What is she going to do next?’ Not, ‘She can’t do this.’”

Annie Banas, MSN, CNP, Clinical Coordinator for PCAVS, helped establish the center 15 years ago with the idea of all services being available at one site. “Our clinic is unique because it functions as both a medical and surgical home for our patients,” she says. “The main pediatric teams involved are ENT, pulmonary medicine and gastroenterology. We also have social work, nutrition, speech pathology and pediatric physiatry.”
PCAVS specializes in helping children like River who have complicated medical histories, says Rachel Georgopoulos, MD, a pediatric otolaryngologist and Director of the Pediatric Endocrine Center. She is the team’s expert for ENT otolaryngology.
“Annie Banas leads the pack, gathering information before and after seeing patients,” Dr. Georgopoulos says. “As the head and neck surgeon, my role is to take care of anyone with airway and breathing issues, loss of hearing and difficulty with feeding. Because River has had such a complicated medical history, she’s the perfect candidate for PCAVS support. She has a trach, swallowing issues, problems with hearing, and was ventilator-dependent. PCAVS provides a multidisciplinary setting.
“It’s amazing how important it is not to work in silos when patients’ medical conditions are this complicated. Even with something as simple as starting a new medication, we have to consider how it will impact their other medical comorbidities and potentially interact with other medications."

“Our team approach supports patients and relieves the impact on families. They don’t have to think about reaching out on their own to individual doctors,” adds Dr. Georgopoulos. “We develop trusting relationships, where there’s a structure of shared decision-making. It’s important to discuss with the family what their goals are — for the patient and for the family.”
Annie Banas concurs. “What is nice about our clinic is that affords us the opportunity to learn the family’s dynamics and have a closer relationship with them and our patients.”
In January 2024, the Kellys faced new challenges when River’s father, Steven, was transferred to Fort Sam Houston in San Antonio, Texas, where he serves as a combat engineer. The PCAVS team helped with River’s transition to new medical providers by compiling a detailed record of her clinical history.
“PCAVS, cardiology and complex care worked together to put together a large binder all about River, her diagnoses and procedures,” Ashley says. “Anything that anyone would need to know about her medical history is all in that book.”
In addition, the PCAVS team recommended some medical experts in their new location before the family moved. “We ended up going with the military doctors,” Ashley says. “But PCAVS also said that if we needed to communicate with them, we could.” River recently was diagnosed with a cyst on her brain and will have surgery in Texas. However, Ashley says, “I know that if I called PCAVS today, they would help.”
Annie says that she and the team miss the Kelly family. “We became friends, and it was hard to let them go and say goodbye. What’s difficult about my job is that I become very empathetic for these families. I can’t imagine navigating a medical system alone. I would advise families with children who need complex care to find a medical team that will listen to them and help coordinate their child’s care.”
At 2 ½ years old, River is making progress, Ashley says. “We weaned her off her oxygen vent settings. She doesn’t walk yet, but she has a walker and a gait trainer. She is still on a feeding tube, getting nothing by mouth, but she will get where she needs to be.”
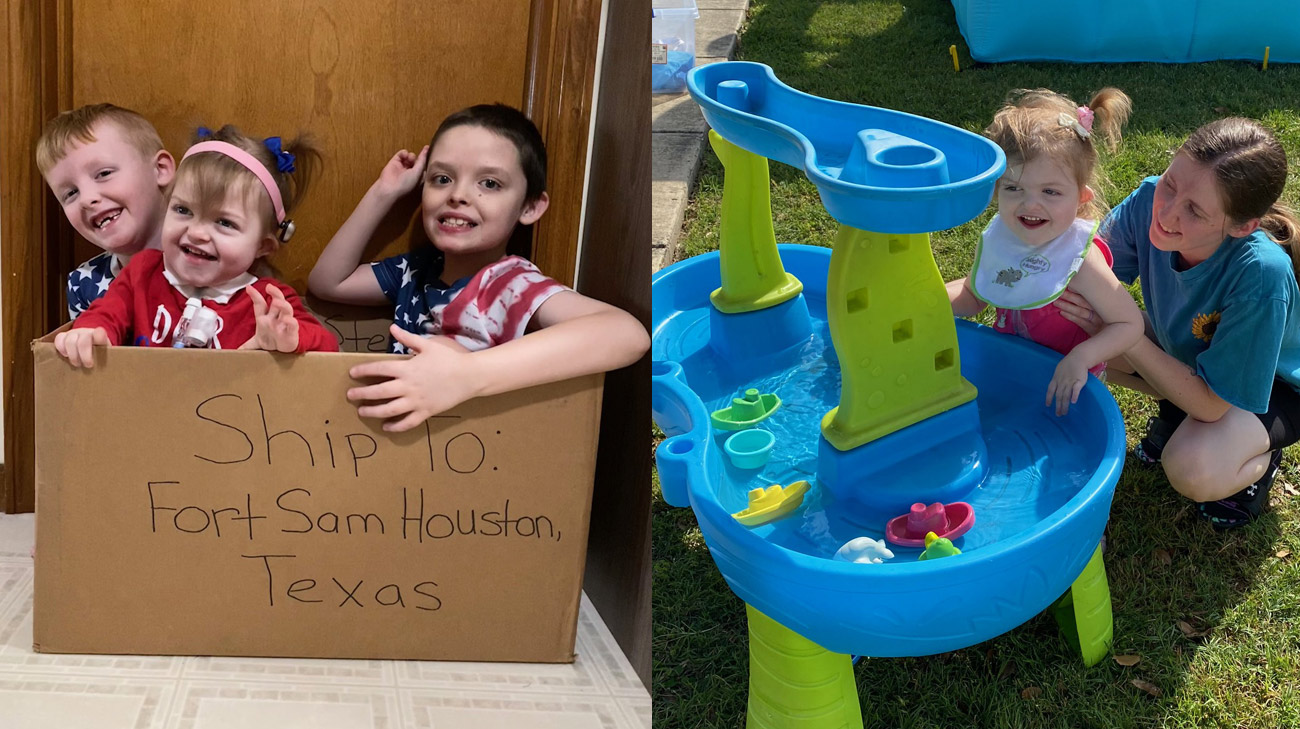
River loves spending time with her brothers, Finn, 7, and Brayson, 9.
“When River was in the hospital for such a long time, it was really hard for our sons because I was always with her. But now, Finn could tell you all the meds she’s on and her daily routines. He knows it all and is so good with her. Brayson and River have a special connection that no one could compete with.”
Eventually, Ashley says, she hopes that her family can return to Cleveland and reunite with the PCAVS team. She adds that her experiences have taught her a valuable lesson. “Never stop advocating for your child,” she says. “You are their voice.”
Related Institutes: Cleveland Clinic Children's

