Botox, or onabotulinumtoxinA, is an FDA-approved treatment to prevent chronic migraines. It works by calming overactive nerves and blocking pain signals. It may lower how many migraines you have and the severity. Injections go in your head, neck and shoulders. Side effects are usually mild and temporary.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Botox for migraines (onabotulinumtoxinA) is a type of botulinum toxin that may prevent chronic migraines. Your provider may recommend it if you have 15 or more headache days per month.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As the drug name is a mouthful, many people just call it by its brand name, Botox®.
While Botox is widely known for cosmetic use, it has medical benefits, too. It may reduce the number and severity of migraines. You’ll get injections in your head, neck and shoulders every 12 weeks (or as recommended).
Your provider will let you know if this treatment is right for you.
Botox works by blocking pain signals before they reach your brain. During a migraine, certain nerves become highly active.
To prevent this, your provider injects Botox into specific muscles in your head, neck and shoulders using a tiny needle. These areas connect to the nerves that send pain signals during a migraine. Botox travels along these connected nerves toward your brainstem. It blocks the release of chemicals that trigger pain.
Botox helps calm any overactive nerves to stop the release of pain signals. This may reduce how often you get a migraine or make symptoms less severe when one happens.
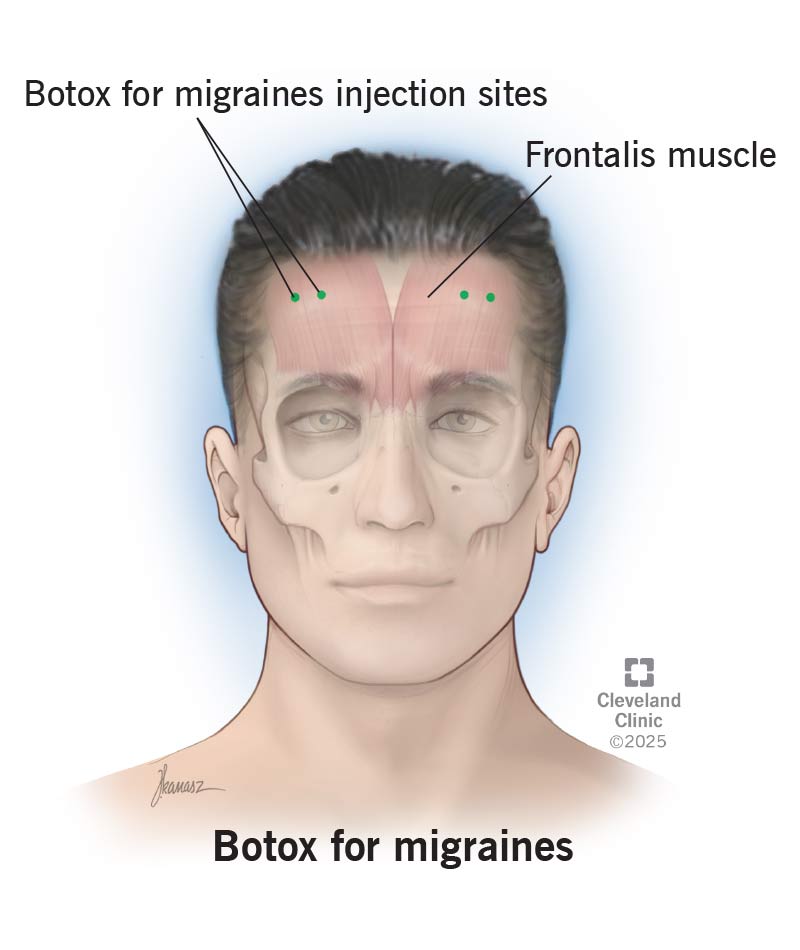
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/botox-for-migraines)
Before your Botox for migraine treatment, you’ll meet with your provider. They’ll explain the risks and benefits and make sure it’s a safe option for you. If you agree to move forward with the treatment, you’ll sign a consent form.
Advertisement
Let your provider know about any medications and supplements you currently take. Botox may interact with different types, like muscle relaxants, for example.
There’s not much that you need to do to prepare. Keep the following in mind on the day of your treatment:
You’ll get 31 small injections in seven different muscles. Your provider will inject them into the following areas:
On the day of your treatment, your provider will:
Most people describe the treatment as a quick pinch or sting. But this really depends on your pain tolerance. The needle that your provider will use is tiny. Keep in mind that they do need to make several pokes in your skin.
Speak up if you’re uncomfortable or if you need a break at any time.
This treatment usually takes between 15 and 20 minutes. It’s done in your healthcare provider’s office. You don’t need to take off the entire day of work or school for it. You can drive yourself to and from your appointment. It’s recommended that you don’t lie down for four hours after receiving Botox.
Side effects of Botox for migraines may include:
These are usually minimal and clear up quickly. Let your provider know if you have any severe pain or discomfort.
The main benefits are that it reduces:
Other benefits may include:
To make sure Botox stays where it’s supposed to, don’t do the following after treatment:
Advertisement
Don’t stop taking your regular migraine medication as prescribed. Your provider will let you know if you need to make changes to your usual migraine medications while participating in Botox injections.
Botox needs time to start working. You should feel the effects after one to two weeks.
It’s normal for the first two cycles of injections not to offer as much relief. Your body is getting used to it. Your provider may recommend two to three rounds of injections. Then, they’ll check to see how well it works. Your provider will make a follow-up appointment after three rounds to determine your long-term treatment plan.
During your injections, it helps to keep track of your migraine symptoms in a headache diary. You can share this with your provider so they know what’s going on between appointments.
The effects of Botox typically last between 10 and 12 weeks. You might notice migraine symptoms coming back as you get closer to your next appointment. Your provider may recommend that you get injections every 12 weeks to keep symptoms away.
You may need Botox injections regularly for a few years to manage symptoms. Your provider may space out the timing of your injections or stop treatments if you notice that you don’t have migraine symptoms anymore. Everyone’s treatment plan is different, so your provider will let you know what will work best for your situation.
Advertisement
Give your provider a call if you have symptoms that don’t improve, like:
Let your provider know if you’re planning to start a family, pregnant or if you’re breastfeeding. Botox isn’t approved during pregnancy or while breastfeeding. There may be other migraine treatment options to help you during this time. Your provider can help you choose the right one.
Yes, it’s possible. But your provider needs to approve it. Getting too much Botox too close together can cause side effects, or your body might stop responding to it over time. You may need to space out the dates between cosmetic and migraine treatments.
If you’re dealing with frequent migraines, you’ve probably tried a lot of things to find relief. And the idea of getting poked in the head and neck every 12 weeks might sound like a hard pass. But for many people with chronic migraines, Botox may be a big help.
Appointments are quick, and the side effects are usually minimal. Over time, you might not need to get poked as often if your symptoms improve. Let your provider know if you have any questions before you get started with this treatment.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Do you have headaches that won’t go away? Or ones that come back regularly? Cleveland Clinic’s headache and migraine experts are here to help.
