Hemorrhoid banding is a procedure to treat internal hemorrhoids. It involves a healthcare provider placing a rubber band at the base of a hemorrhoid to cut off its blood supply. Your provider can do the procedure in their office.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
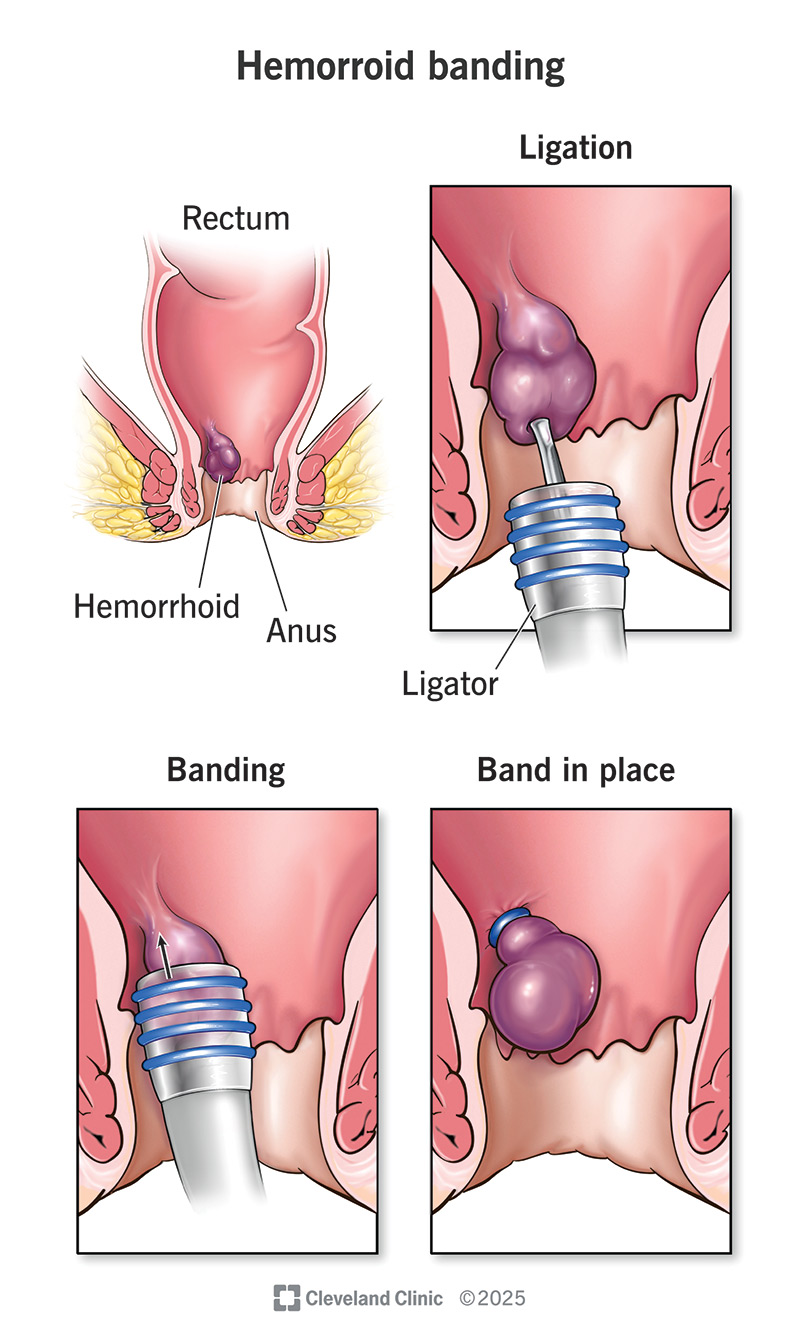
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/hemorrhoid-banding.jpg)
Hemorrhoid banding (rubber band ligation) is a treatment to shrink internal hemorrhoids. Hemorrhoids are swollen veins inside your rectum. They can cause symptoms like rectal bleeding, pain and itching.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The procedure involves your healthcare provider placing a rubber band around the base of the hemorrhoid, cutting off its blood supply. Without blood, the hemorrhoid shrinks and falls off.
Your healthcare provider may recommend a rubber hand ligation if:
The procedure is only used for internal hemorrhoids and may not work for large hemorrhoids.
Your healthcare provider may give you instructions to follow before the procedure. It could include information about:
Your provider may do one last examination of the hemorrhoid(s) before the banding procedure.
Here is what you can expect from hemorrhoid banding:
Advertisement
The procedure takes less than five minutes. If you have several hemorrhoids, you may need a follow-up appointment to treat them. Your provider may only treat one or two hemorrhoids with banding at a time.
The rubber band cuts off the hemorrhoid’s blood supply. This causes it to shrivel up and fall off, usually within one week. A scar will form where the hemorrhoid was.
Some other things you can expect after are:
You can usually go back to your usual activities right after hemorrhoid banding. Some people need to take it slow for a day or two.
You poop normally after the procedure. Your healthcare provider may recommend ways to soften your stool to make bowel movements easier. This could include eating more fiber, drinking lots of water or using medication to soften your poop.
Hemorrhoid banding is a good option for shrinking internal hemorrhoids without surgery. Your provider can do it in their office. The recovery is also quick compared to other treatments for hemorrhoids.
It’s generally successful, but factors like the size and severity of the hemorrhoid play a role. Most studies find it to be between 70% and 80% effective.
Complications are rare but could include:
There’s a chance that the treatment won’t work. If this is the case, your provider will recommend other options to remove internal hemorrhoids.
Recovery is usually quick. You may find it hard to poop or have excessive gas for the first few days. Here are some things you can do to help with your recovery:
No one wants to live with hemorrhoids. They can interfere with your quality of life and cause you discomfort. If you have internal hemorrhoids that don’t go away with at-home treatment, hemorrhoid banding may be an option for you. Talking to your provider about hemorrhoids can be an awkward conversation, but it’s necessary if you want to feel relief from your symptoms. Ask them if hemorrhoid banding is an option for you and what you can expect from this treatment.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When hemorrhoids cause pain or bleeding, you want the best possible care. Cleveland Clinic’s providers can make you more comfortable with a variety of treatments.
