Cushing syndrome is a condition caused by too much cortisol in your body. It can happen because of medications or a tumor on your pituitary or adrenal glands. Common symptoms are weight gain and skin changes. There are treatments to lower cortisol and improve symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cushing syndrome is a rare hormonal condition that happens when your body has too much cortisol. Cortisol is an important hormone that controls many bodily functions. But having too much of it can cause symptoms, like a round or full face, weight gain and skin changes. The most common causes of Cushing syndrome are taking corticosteroid medications or developing a tumor on your pituitary or adrenal glands.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Treatment focuses on lowering cortisol levels.
You may also hear this condition called hypercortisolism or Cushing’s syndrome.
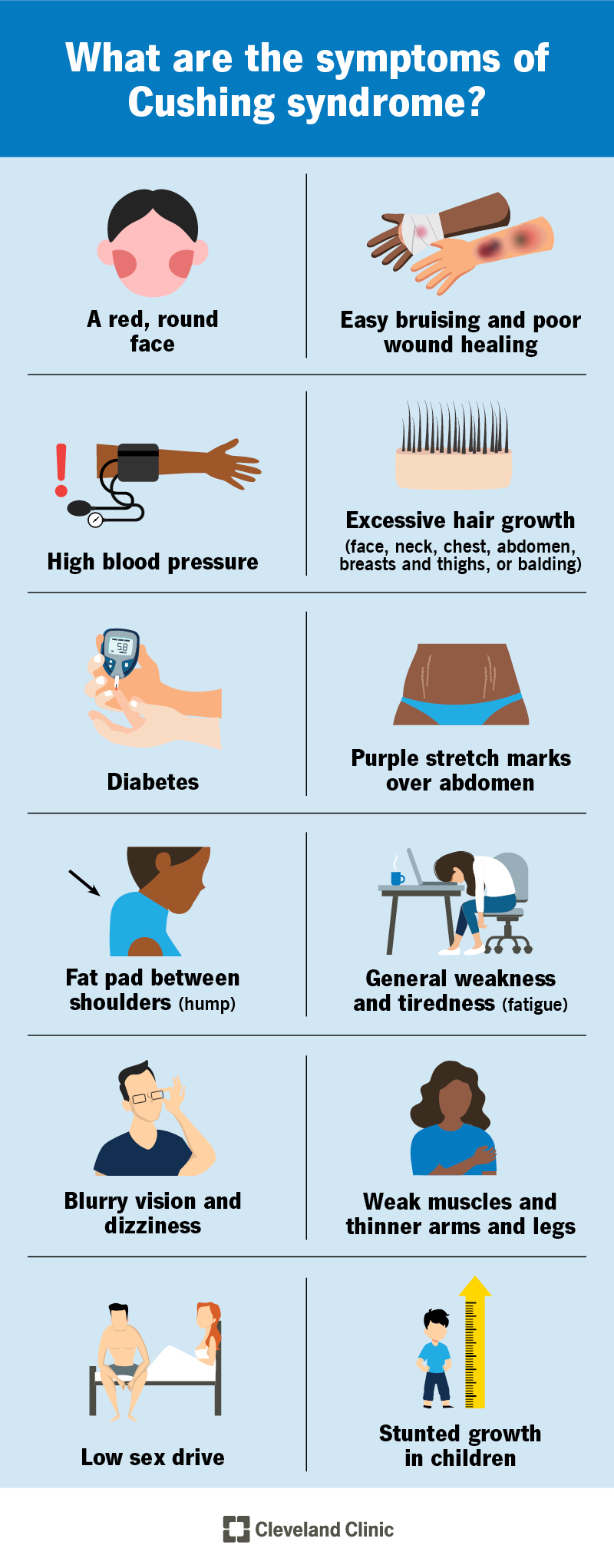
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/5497-cushing-syndrome)
Signs and symptoms of Cushing’s can vary. You may have one, many or none of the following signs:
Other symptoms could include:
Too much cortisol causes Cushing syndrome. The causes can come from two different sources:
Several factors can lead to high cortisol levels, including:
Advertisement
Anyone can develop Cushing syndrome. But it’s more likely to affect women and people between 25 and 50 years old.
Without treatment, hypercortisolism can cause health problems, including:
If left untreated, Cushing syndrome can result in death. This is mainly because of complications related to diabetes or cardiovascular diseases.
Your healthcare provider will ask questions about your symptoms, look at your medical history and do a physical exam. They’ll order tests that check cortisol and other hormone levels.
Cushing’s can be difficult to diagnose. This is because some of its symptoms, like tiredness and weight gain, can have several other causes.
Your healthcare provider may order the following tests:
Once your provider diagnoses the condition, they’ll figure out the underlying cause. If you don’t take glucocorticoids, it usually points to a tumor.
Your provider may recommend the following imaging tests to find the tumor:
Cushing’s treatment depends on the underlying cause of high cortisol levels. If you use glucocorticoids, your healthcare provider will lower the dosage or prescribe a different medication. Your provider will carefully evaluate the situation and work on lowering the dose slowly without causing you harm.
If a tumor is causing Cushing syndrome, your provider may suggest surgery or radiation, depending on the location and other factors.
Another option is for your healthcare provider to prescribe a medication that slows down cortisol production.
Treatment depends on the underlying cause. Options include:
Advertisement
Cushing syndrome can get worse without proper treatment. Have regular checkups with your healthcare provider. Let them know of any new or worsening symptoms.
In many cases, treatment will cure Cushing syndrome and improve your symptoms.
You may feel embarrassed by some of the symptoms this disease causes. If it’s taking a toll on your mental health, reach out to a therapist. Joining a support group of others living with the condition may help, too. Your mental health is just as important as your physical health.
It can be life-threatening without treatment. This is mostly because of the strain it can put on your heart and endocrine system. With the right treatment, your life expectancy shouldn’t be affected.
From rapid weight gain to skin changes, Cushing syndrome can drastically change your body. It can be hard on your mental health, as well. But with the right treatment, Cushing syndrome can be cured. Stay in contact with your healthcare provider during every stage. Follow their instructions and don’t hesitate to ask questions. Lean on loved ones for support, too.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Finding out you have Cushing disease can end years of wondering about your symptoms. Cleveland Clinic is here to help you get the diagnosis and treatment you need.
