Smith-Magenis syndrome is a developmental condition caused by a chromosome deletion. The condition affects your child’s ability to fall asleep and stay asleep, their ability to learn and their behavior. There’s no cure for Smith-Magenis syndrome, but treatment is supportive of symptoms that affect your child.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Smith-Magenis syndrome is a developmental condition that affects several parts of your child’s body. Some of the main symptoms include abnormal cognitive development (intellectual disability), unique facial features, behavioral concerns and difficulty sleeping. Smith-Magenis syndrome occurs because a small piece of a chromosome, carrying an important gene, is deleted from your child’s DNA during embryonic development.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Smith-Magenis syndrome can affect anyone, as the genetic change occurs at the time of conception when the egg and sperm meet. There’s usually no history of the condition in your biological family line. This is known as a spontaneous or “de novo” mutation.
In rare cases, your child may inherit the condition from a biological parent who doesn’t have symptoms of the condition but has a genetic change in some of their sex cells but not all of their cells. This type of inheritance is called germline mosaicism.
Smith-Magenis syndrome affects 1 out of every 15,000 to 25,000 people worldwide.
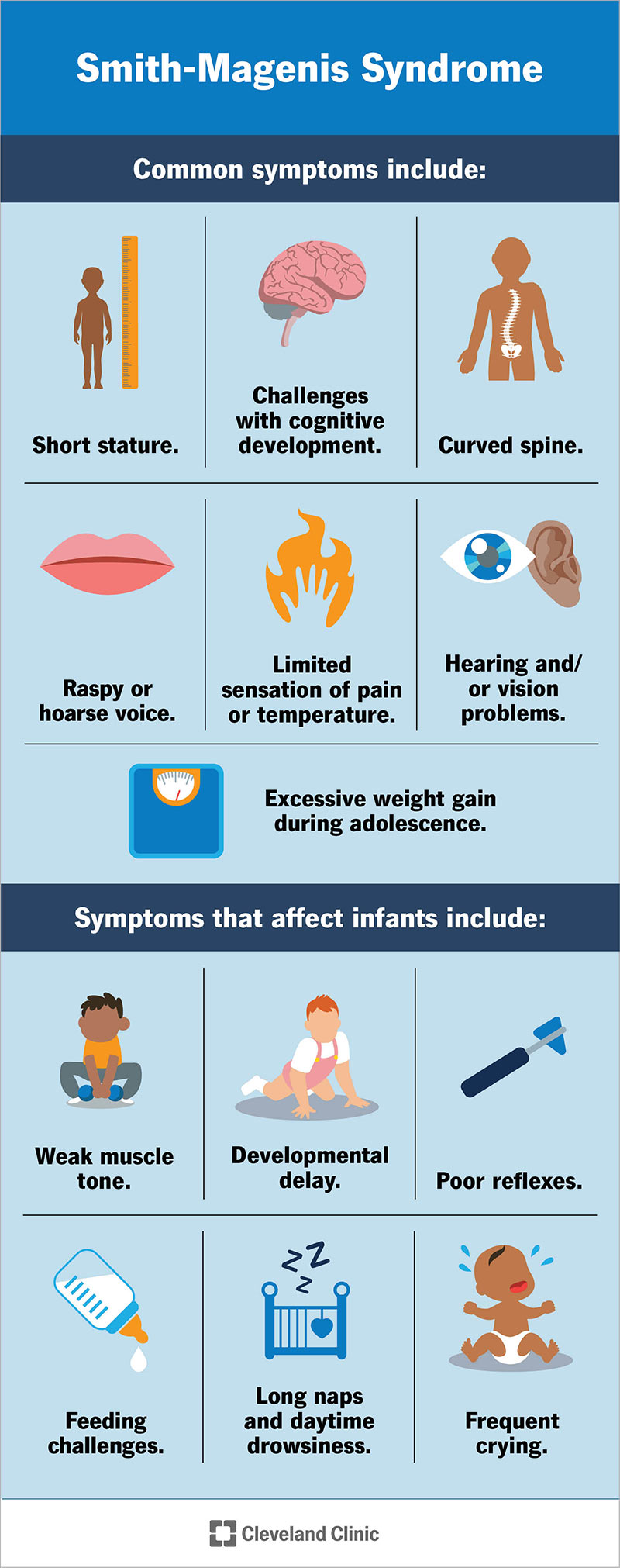
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24467-smith-magenis-syndrome)
Symptoms of Smith-Magenis syndrome affect multiple organ systems in your child’s body. They range in severity from mild to severe. Common symptoms include:
Symptoms that affect infants include:
Although rare, severe cases of Smith-Magenis syndrome can affect the function of your child’s heart and kidneys. It can also cause seizures.
Advertisement
People born with Smith-Magenis syndrome have characteristic facial features that become more apparent during middle childhood. These features include:
Some children and adults diagnosed with Smith-Magenis syndrome have dental abnormalities due to their facial structure.
Smith-Magenis syndrome can make sleeping difficult for infants, children and adults diagnosed with the condition. Sleep disturbances include:
The change in sleep patterns relates to melatonin secretion in individuals with Smith-Magenis syndrome.
Children diagnosed with Smith-Magenis syndrome can display certain emotional or behavioral symptoms, including:
They may also have conditions that affect their behavior like ADHD or autism spectrum disorder.
Changes to the retinoic acid-induced 1 gene (RAI1) cause Smith-Magenis syndrome. The RAI1 gene is responsible for producing proteins that give your cells instructions to do their job throughout your body. This gene isn’t completely understood, but studies suggest that this gene creates proteins for several parts of your child’s body, which is why symptoms of Smith-Magenis syndrome are so broad.
A chromosome deletion (a portion containing the RAI1 gene) or a mutation of the RAI1 gene itself causes Smith-Magenis syndrome. Nearly 90% of children diagnosed with the condition are missing the RAI1 gene, which is part of the short arm (p) of chromosome 17 (17q11.2).
The chromosome deletion is spontaneous (de novo) and happens randomly when the egg and sperm meet at conception. In very rare cases, chromosomes from the egg and sperm break apart and trade places with each other (translocation). These rare cases happen very early during the development of an embryo. The remaining 10% of those diagnosed have a genetic mutation of the RAI1 gene, which causes a change in the structure of the child’s DNA at that specific gene location.
A diagnosis of Smith-Magenis syndrome usually occurs during childhood when symptoms become more apparent. Your child’s provider will ask questions to learn more about their symptoms, take a complete medical history and examine your child. A genetic blood test is necessary to confirm a diagnosis and rule out similar conditions.
Treatment for Smith-Magenis syndrome focuses on relieving symptoms of the condition, which could include:
Advertisement
Your child’s provider will individualize their treatment to fit your child’s needs to help them thrive.
Your child will likely need a team of medical professionals to treat symptoms of Smith-Magenis syndrome that affect different parts of their body. Their care team could consist of:
Melatonin is a hormone within your body that helps you go to sleep. Melatonin supplements can help your child fall asleep and regulate their sleep-wake cycle. If your child has trouble sleeping because of Smith-Magenis syndrome, melatonin supplements can help them get a better night’s sleep if they take the supplement before bed. If your child has trouble sleeping, talk to their provider to make sure melatonin supplements are right for them.
The prognosis for Smith-Magenis syndrome is dependent on the severity of your child’s symptoms. Some people diagnosed with the condition have a normal life span and can live semi-independently with limited support from their family, friends and caregivers. Others might need more support throughout their entire life and benefit from living in a group setting or a residential care community. Symptom management and preventative care is lifelong to help your child live a healthy and full life.
Advertisement
No, there isn’t a cure for Smith-Magenis syndrome. The condition occurs randomly due to changes to your child’s DNA. Your child’s provider will offer individualized treatment options to help with symptom management throughout your child’s life span.
You can’t prevent Smith-Magenis syndrome because the condition is genetic. Changes to your child’s DNA happen randomly and unpredictably. Medical, physical and behavioral interventions are available to help your child manage their symptoms and live a full life.
Visit your child’s healthcare provider if your child:
Visit the emergency room if your child:
It can be difficult to learn that your child has a developmental condition that affects several parts of their growing body. Many parents and caregivers find comfort in participating in support groups for Smith-Magenis syndrome. Your child’s provider will offer management options for their symptoms to help your child reach their fullest potential. While there isn’t a cure for Smith-Magenis syndrome, lifelong support is available through your child’s care team.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your child doesn’t walk, talk or smile as soon as other kids, you may worry. Cleveland Clinic Children’s offers personalized treatment for developmental delays.
